Hormones play a vital role in regulating male reproductive function. From sperm production to sexual performance and libido, the male endocrine system must remain in delicate balance to support fertility. However, even slight disruptions in hormone levels can lead to impaired testicular function, poor sperm quality, and difficulties in achieving pregnancy.
Hormonal imbalances are often overlooked as a cause of male infertility, yet they may be reversible when properly diagnosed and treated. In this comprehensive guide, we’ll explore the role of hormones in male fertility, what happens when those hormones are out of balance, and how to restore healthy reproductive function through medical and lifestyle interventions.
Understanding the Role of Hormones in Male Fertility
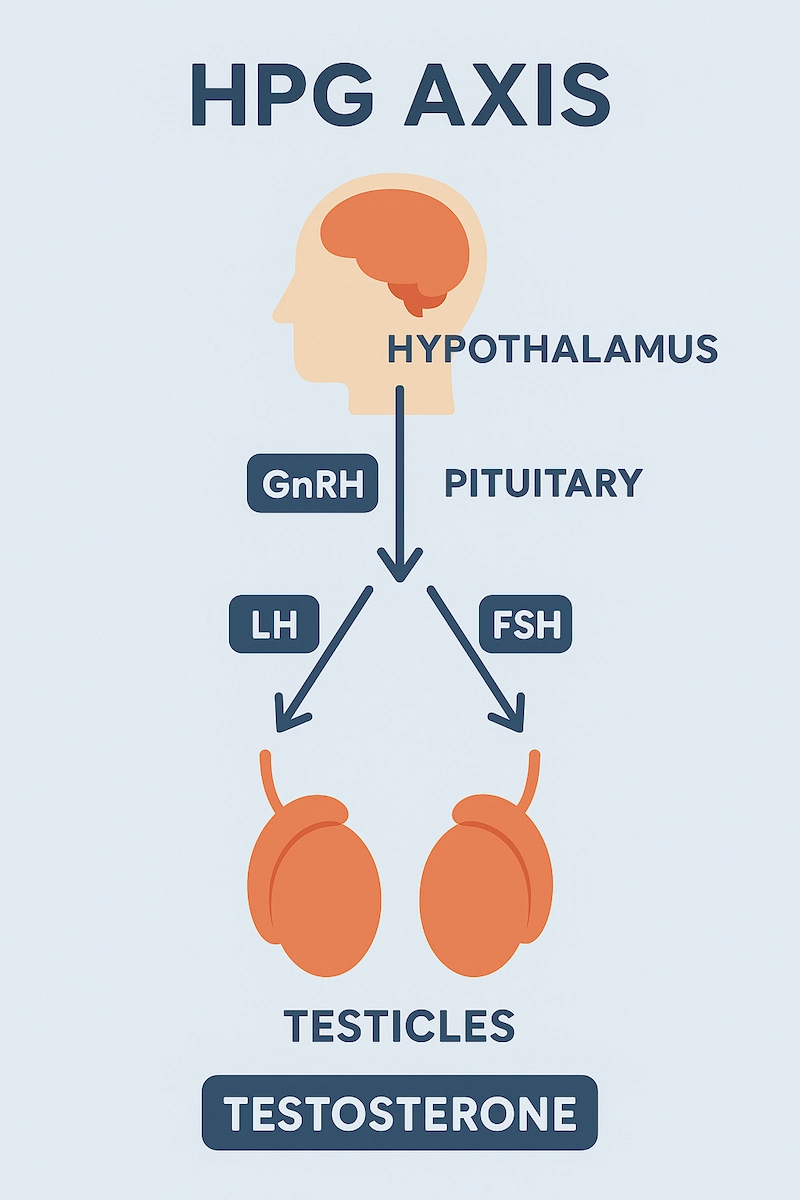
Hormones are essential messengers that regulate nearly every aspect of male reproductive function, including sperm production, sexual drive, and testicular health. These hormones operate through a tightly coordinated system known as the hypothalamic-pituitary-gonadal (HPG) axis.
The Hypothalamic-Pituitary-Gonadal (HPG) Axis
The HPG axis is a feedback loop involving the hypothalamus, pituitary gland, and testes. This axis controls the production and regulation of the main reproductive hormones in men:
- Gonadotropin-releasing hormone (GnRH) – Produced by the hypothalamus, GnRH signals the pituitary gland to release two key hormones: LH and FSH.
- Luteinizing hormone (LH) – Stimulates the Leydig cells in the testes to produce testosterone, the primary male sex hormone.
- Follicle-stimulating hormone (FSH) – Acts on the Sertoli cells to support spermatogenesis, the process of sperm cell development.
- Testosterone – Plays a critical role in sperm production, sexual function, muscle mass, bone density, and libido.
This hormonal system functions through negative feedback: when testosterone levels are sufficient, the hypothalamus and pituitary reduce their signaling. When testosterone is low, they increase their hormonal output to stimulate the testes.
🔄 Hormonal Balance and Fertility
For sperm production and male fertility to remain optimal, the levels of LH, FSH, and testosterone must be within a narrow physiological range. An imbalance at any level of the HPG axis can disrupt this system, leading to:
- Reduced or halted sperm production
- Poor sperm motility or morphology
- Erectile dysfunction or reduced libido
- Hormonal suppression due to external factors (e.g., anabolic steroids)
Even small shifts in hormone levels can have significant effects on fertility, especially if they go undetected over time.
Key Takeaway
Male fertility is not just about sperm count—it depends on a complex hormonal interplay. Understanding this system is the first step toward identifying and treating infertility linked to hormonal imbalance.
Common Hormonal Imbalances That Affect Male Fertility
Several hormonal imbalances can impair male fertility by disrupting testosterone production, reducing sperm quality, or affecting sexual function. Identifying the specific type of imbalance is crucial for targeted treatment and fertility restoration.
1. Low Testosterone (Hypogonadism)
Low levels of testosterone—also known as male hypogonadism—can lead to decreased sperm production, reduced libido, fatigue, and erectile dysfunction. Hypogonadism is classified as:
- Primary hypogonadism: Testicular failure (low testosterone with high LH/FSH)
- Secondary hypogonadism: Pituitary or hypothalamic dysfunction (low testosterone with low LH/FSH)
- Mixed hypogonadism: Involves both primary and secondary mechanisms
Testosterone is essential for spermatogenesis, so any drop below normal physiological levels can significantly reduce fertility.
2. High Estrogen (Estradiol Dominance)
While men produce small amounts of estradiol, excess levels can inhibit the HPG axis through negative feedback, suppressing LH and FSH production. This leads to lower testosterone and reduced sperm output.
High estrogen is often associated with:
- Obesity (via increased aromatase activity)
- Liver dysfunction (impaired estrogen clearance)
- Environmental exposure to xenoestrogens (e.g., plastics, pesticides)
3. Elevated Prolactin (Hyperprolactinemia)
Prolactin is primarily known for its role in female lactation, but elevated levels in men can suppress GnRH release, leading to low LH, FSH, and testosterone.
Common causes:
- Pituitary tumors (prolactinomas)
- Medications (e.g., antipsychotics, antidepressants)
- Hypothyroidism
Symptoms may include infertility, low libido, erectile dysfunction, and gynecomastia (breast enlargement).
4. Low FSH or LH Levels
Low levels of FSH and/or LH impair the stimulation of the testes, leading to poor sperm production and low testosterone. This may result from:
- Pituitary dysfunction
- Excessive stress or energy deficiency
- Use of anabolic steroids or exogenous testosterone
These cases are often classified under secondary hypogonadism.
5. Thyroid Hormone Imbalances
Both hypothyroidism and hyperthyroidism can affect male fertility:
- Hypothyroidism: Can lower testosterone, reduce libido, and increase prolactin
- Hyperthyroidism: Can impair sperm motility and cause testicular discomfort
Correcting thyroid function often leads to a reversal of fertility issues.
6. Insulin Resistance and Metabolic Syndrome
Conditions like type 2 diabetes, obesity, and metabolic syndrome are associated with low testosterone, increased estrogen, and oxidative stress—all of which negatively impact sperm quality and hormone regulation.
Lifestyle modifications and improved insulin sensitivity can help rebalance reproductive hormones.
Causes of Hormonal Imbalances in Men
Hormonal imbalances affecting male fertility can arise from a variety of internal (endogenous) and external (exogenous) factors. Understanding these causes is essential for accurate diagnosis, prevention, and treatment.
1. Genetic or Congenital Disorders
Certain inherited conditions can disrupt hormone production or signaling, including:
- Klinefelter syndrome (47,XXY): A chromosomal disorder leading to small testicles, low testosterone, and infertility
- Kallmann syndrome: Delayed or absent puberty due to GnRH deficiency
- Androgen insensitivity syndrome: Defective androgen receptors cause resistance to testosterone
These conditions are usually diagnosed during adolescence or early adulthood.
2. Pituitary Gland Disorders
The pituitary gland regulates LH and FSH, which are essential for testosterone and sperm production. Disorders that affect the pituitary may include:
- Pituitary tumors (e.g., prolactinoma)
- Trauma or surgery near the brain
- Radiation therapy to the head
- Infections or inflammation (e.g., hypophysitis)
Such conditions often lead to secondary hypogonadism and may require hormonal or surgical treatment.
3. Obesity and Excess Body Fat ⚖️
Excess adipose tissue increases aromatase activity, which converts testosterone into estrogen, leading to estrogen dominance and suppressed testosterone production.
Additionally, obesity is associated with:
- Insulin resistance
- Leptin dysregulation
- Increased oxidative stress — all of which can impair reproductive hormones and sperm quality
4. Chronic Stress and Cortisol Dysregulation 😫
Long-term stress leads to elevated cortisol, which interferes with the HPG axis and can suppress GnRH, LH, and testosterone. Stress is also linked to:
- Poor sleep quality
- Reduced libido
- Mood disorders — which can indirectly impact fertility
5. Anabolic Steroid or Exogenous Testosterone Use 💉
Using anabolic steroids or testosterone therapy for bodybuilding or anti-aging can shut down natural testosterone production via negative feedback on the HPG axis. This results in:
- Testicular shrinkage (atrophy)
- Low sperm count or azoospermia
- Long-term hormonal suppression even after stopping use
- This is a major preventable cause of infertility in otherwise healthy men.
6. Liver or Kidney Disease
Both the liver and kidneys help metabolize and clear hormones from the bloodstream. Chronic liver or kidney dysfunction can lead to:
- Elevated estrogen
- Altered SHBG (sex hormone-binding globulin) levels
- Disrupted testosterone balance
These conditions often affect multiple hormone systems, not just the reproductive axis.
7. Environmental Endocrine Disruptors
Exposure to certain chemicals may interfere with hormone production or receptor function. These include:
- Phthalates (in plastics, personal care products)
- Bisphenol A (BPA)
- Pesticides and herbicides
- Heavy metals (lead, cadmium)
Minimizing exposure to these substances can support hormonal health and fertility.
Signs and Symptoms of Hormonal Imbalance in Men
Hormonal imbalances often develop gradually and may go unnoticed until they begin to impact fertility or overall well-being. Recognizing the signs early can lead to faster diagnosis and more effective treatment.
1. Low Libido and Erectile Dysfunction 🍃
One of the most common signs of low testosterone is a reduced sex drive (libido). Men may also experience:
- Difficulty achieving or maintaining erections
- Reduced sexual satisfaction
- Delayed ejaculation or anorgasmia
These symptoms often overlap with psychological factors like stress or anxiety, but a hormonal component should always be considered.
2. Fatigue and Low Energy 🔋
Testosterone supports energy metabolism, red blood cell production, and stamina. Men with hormonal imbalances frequently report:
- Chronic tiredness
- Reduced motivation
- Poor exercise tolerance
- Feeling “burned out” despite rest
Fatigue can also be a symptom of thyroid or cortisol dysregulation.
3. Mood Swings and Depression 😔
Low testosterone and abnormal prolactin or thyroid hormone levels are linked to depressed mood, irritability, and emotional instability. Some men may experience:
- Difficulty concentrating
- Increased anxiety
- Loss of interest in daily activities (anhedonia)
Hormonal testing is often overlooked in men with mental health symptoms.
4. Loss of Muscle Mass and Increased Body Fat 💪➡️⚖️
Testosterone helps build and maintain lean muscle mass. Men with low levels often notice:
- Decreased strength and endurance
- Difficulty gaining or maintaining muscle
- Accumulation of fat, particularly around the abdomen
This change in body composition can also reinforce hormonal imbalance through increased estrogen production from fat tissue.
5. Reduced Testicle Size or Firmness
Testicular atrophy (shrinkage) may result from:
- Long-standing low LH/FSH stimulation
- Exogenous testosterone use
- Elevated estrogen levels
This is often subtle but may be noted during physical exam or self-checks.
6. Fertility Issues 👶
Men with hormonal imbalances frequently experience:
- Low sperm count (oligospermia)
- Poor motility or morphology
- Azoospermia (no sperm in semen)
- Difficulty conceiving after 12+ months of unprotected intercourse
In many cases, this is the first sign that leads to hormonal evaluation.
7. Gynecomastia (Breast Enlargement)
Excess estrogen or an imbalance between estrogen and testosterone can lead to breast tissue growth in men, often accompanied by tenderness or swelling.
Diagnostic Evaluation for Hormonal Imbalances
Accurately diagnosing a hormonal imbalance is essential for identifying the root cause of male infertility and guiding effective treatment. The diagnostic process includes a combination of medical history, physical examination, laboratory tests, and sometimes imaging studies.
1. Medical History and Physical Examination
A thorough medical and reproductive history is the foundation of hormonal evaluation. Key topics include:
- Duration of infertility
- Changes in libido or sexual function
- History of anabolic steroid use or testosterone therapy
- Past illnesses, head trauma, or pituitary disorders
- Medications (e.g., antipsychotics, antidepressants)
- During the physical exam, the doctor may assess:
- Testicular size, firmness, and symmetry
- Signs of gynecomastia
- Body fat distribution
- Muscle mass and hair pattern (linked to testosterone activity)
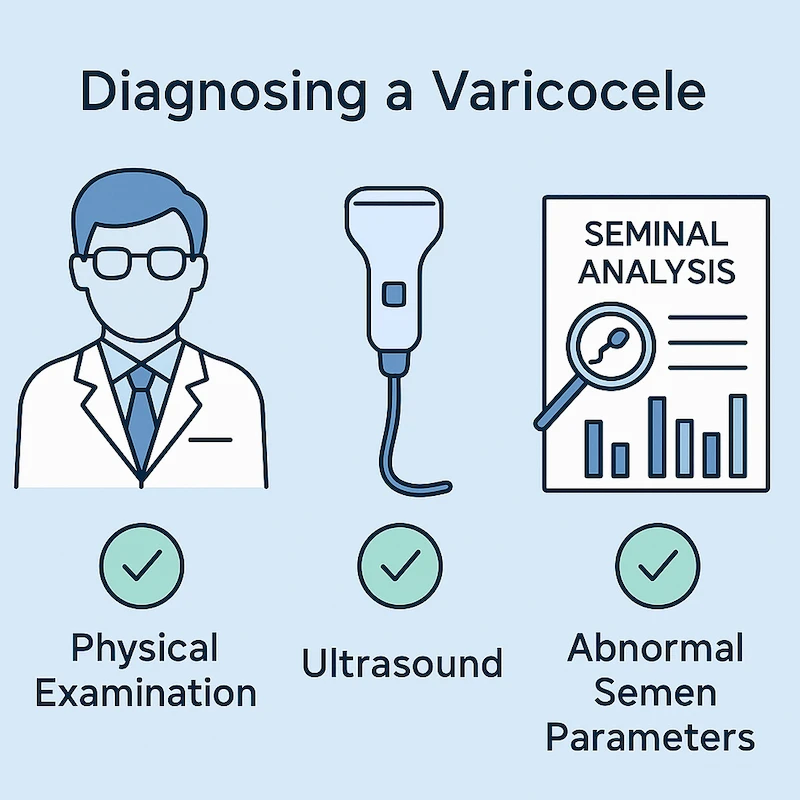
2. Semen Analysis
While not a hormone test, semen analysis is crucial to evaluate the functional impact of hormonal imbalance. Findings may include:
- Low sperm count (oligospermia)
- No sperm (azoospermia)
- Poor motility or morphology
If semen parameters are abnormal, hormonal testing is typically the next step.
3. Hormonal Blood Tests 🩸
Blood tests are used to assess hormone levels and determine whether the issue lies in the testes, pituitary, or hypothalamus. Common tests include:
- Total testosterone (drawn in the morning, when levels peak)
- Free testosterone (more accurate in cases of altered SHBG)
- LH (luteinizing hormone) – Helps determine if the problem is primary or secondary
- FSH (follicle-stimulating hormone) – Important for evaluating spermatogenesis
- Estradiol (E2) – To detect estrogen excess
- Prolactin – Elevated levels may suppress GnRH
- TSH, Free T3, Free T4 – To rule out thyroid disorders
- SHBG (sex hormone-binding globulin) – Affects total vs. free testosterone levels
These tests are often ordered together as part of a male fertility or hypogonadism panel.
4. Imaging Studies 🧠
Imaging is not always required but may be indicated in certain cases:
- Pituitary MRI: Recommended if prolactin is significantly elevated or if there are signs of pituitary dysfunction (e.g., vision changes, headaches)
- Scrotal ultrasound: May be used to evaluate testicular size, atrophy, or underlying structural issues like varicocele
5. Genetic Testing (When Indicated)
In cases of non-obstructive azoospermia or suspected congenital causes (e.g., Klinefelter syndrome), genetic tests may be recommended:
- Karyotype analysis
- Y chromosome microdeletion testing
- CFTR mutation screening (in suspected congenital absence of the vas deferens)
Treatment Options for Hormonal Imbalances
The treatment of hormonal imbalances in men depends on the underlying cause, the severity of symptoms, and the goal of therapy—particularly whether the man is trying to conceive. In many cases, restoring hormonal balance can significantly improve sperm quality and overall reproductive function.
1. Lifestyle Modifications 🥦🏃♂️
For mild hormonal imbalances—especially those linked to obesity, stress, or poor sleep—lifestyle changes can be the first and often most effective intervention:
- Weight loss: Reduces aromatase activity and estrogen levels
- Regular exercise: Boosts natural testosterone and improves insulin sensitivity
- Quality sleep: At least 7–8 hours nightly helps regulate the HPG axis
- Stress reduction: Mindfulness, yoga, and stress management can improve hormonal rhythms
- Avoiding alcohol, tobacco, and recreational drugs
These strategies are especially effective in early-stage hypogonadism or metabolic-related hormone disruption.
2. Clomiphene Citrate (Clomid) 💊
Clomiphene is an oral medication that stimulates the hypothalamus to produce more GnRH, thereby increasing LH and FSH. This helps boost endogenous testosterone and stimulate sperm production.
- Often used in secondary hypogonadism or men with low T who wish to maintain fertility
- Alternative to testosterone replacement therapy (TRT), which suppresses sperm production
Typical dosage: 25–50 mg orally every other day (adjusted based on response)
3. hCG Therapy (Human Chorionic Gonadotropin)
hCG mimics LH, stimulating the Leydig cells to produce testosterone naturally. It is often combined with FSH injections in cases of severe infertility or non-obstructive azoospermia.
- Used in men with pituitary suppression or anabolic steroid-induced hypogonadism
- Helps preserve testicular size and sperm output
Dosage varies and is typically injected subcutaneously several times per week.
4. Aromatase Inhibitors (e.g., Anastrozole)
In men with high estrogen (elevated estradiol), aromatase inhibitors block the conversion of testosterone to estrogen.
- Useful in obese men or those with estrogen dominance
- Helps raise testosterone levels and reduce estrogen-driven suppression of LH/FSH
- Used cautiously and under medical supervision
5. Dopamine Agonists for High Prolactin
For men with hyperprolactinemia, especially due to prolactin-secreting pituitary tumors, medications like:
- Cabergoline or
- Bromocriptine
are prescribed to lower prolactin, restore LH/FSH secretion, and normalize testosterone levels.
These drugs often improve both fertility and sexual function.
6. Thyroid Hormone Therapy
Men with hypothyroidism or hyperthyroidism may require:
- Levothyroxine (for underactive thyroid)
- Antithyroid medications (for overactive thyroid)
Correcting thyroid dysfunction usually helps normalize prolactin, testosterone, and sperm motility.
7. Testosterone Replacement Therapy (TRT) – With Caution ⚠️
While TRT can improve symptoms like fatigue and low libido, it suppresses LH and FSH, often worsening fertility by shutting down sperm production.
- Not recommended for men actively trying to conceive
- May be considered only in older men or those with completed fertility plans
- Alternatives (like Clomid or hCG) are preferred for fertility preservation
8. Treating Underlying Conditions
- Pituitary tumors: May require surgery or medication
- Anabolic steroid withdrawal: Requires time and medical support to restore natural function
- Chronic disease management: Optimizing liver, kidney, or metabolic health improves hormonal balance
Hormonal Treatment and Fertility Outcomes
Treating hormonal imbalances can significantly improve male fertility, especially when the underlying cause is diagnosed early and addressed appropriately. Depending on the type of hormonal issue, men may experience noticeable improvements in sperm quality, testosterone levels, and natural conception rates.
Improved Semen Parameters After Treatment
In men with secondary hypogonadism (low testosterone with low LH/FSH), medications like Clomiphene or hCG can stimulate the testes to:
- Increase sperm count (oligospermia → normal range)
- Improve sperm motility and morphology
- Restore ejaculate volume
These changes typically occur within 3 to 6 months, although improvement may take longer in men with more severe hormone suppression.
Recovery from Anabolic Steroid-Induced Infertility
Men who previously used anabolic steroids often present with azoospermia or severely suppressed sperm production. With medical support (e.g., hCG + Clomid), many can recover:
- Sperm return: In 4–12 months, depending on duration of steroid use
- Testicular size and testosterone production may also normalize
- Recovery can be partial or complete, and some cases may require assisted reproduction
Effects on Natural Conception Rates
With appropriate hormonal treatment:
- Spontaneous pregnancy occurs in up to 40–60% of couples (depending on female factors)
- Fertility improvements are best in men with mild to moderate hormone deficiencies
- Hormonal treatment is often more cost-effective and less invasive than immediate ART (IUI/IVF)
Role in Assisted Reproductive Technology (ART)
For men with persistent subfertility despite hormone therapy, ART options may be considered:
- Intrauterine insemination (IUI): If sperm count and motility improve moderately
- In vitro fertilization (IVF) or ICSI: For severe cases or when sperm recovery is incomplete
Even in ART, improved hormonal balance often leads to better sperm quality, higher fertilization rates, and higher live birth outcomes.
Realistic Expectations and Monitoring
- Hormonal treatment requires patience and consistency
- Semen analysis should be repeated every 3 months to monitor progress
- Hormone levels should be tracked regularly to avoid over- or under-treatment
- Some men may need long-term maintenance therapy or lifestyle adjustment
Natural Ways to Support Hormonal Balance and Fertility
While medical treatment may be necessary in many cases, natural approaches can play a powerful supportive role in restoring hormonal health and improving male fertility. These strategies not only enhance the effectiveness of medical therapy but also help prevent recurrence of hormonal imbalances.
1. Optimize Nutrition 🍳🥦
A well-balanced diet rich in essential nutrients helps regulate hormone production and support sperm health. Key fertility-boosting nutrients include:
- Zinc – Supports testosterone synthesis and sperm production (found in oysters, pumpkin seeds, beef)
- Vitamin D – Linked to testosterone and sperm motility (via sunlight, fatty fish, fortified foods)
- Omega-3 fatty acids – Improve sperm morphology and reduce inflammation (found in salmon, flaxseeds, walnuts)
- Selenium – Antioxidant that protects sperm DNA (found in Brazil nuts, tuna)
- Folate and B-vitamins – Important for DNA synthesis in sperm cells
Avoid processed foods, excess sugar, and trans fats, which can worsen insulin resistance and lower testosterone.
2. Maintain a Healthy Weight ⚖️
Obesity is strongly linked to low testosterone, increased estrogen, and reduced fertility. Losing 5–10% of body weight through diet and exercise can:
- Increase natural testosterone levels
- Improve insulin sensitivity
- Enhance sperm quality
Even small improvements in weight can have a meaningful impact on hormonal balance.
3. Exercise Regularly, But Smartly 🏋️♂️
Physical activity improves circulation, metabolism, and testosterone production. Best practices include:
- Strength training (3–4 times/week): Stimulates natural testosterone
- Moderate cardio (e.g., walking, cycling): Supports fat loss and hormonal regulation
- Avoid overtraining: Excessive endurance training can increase cortisol and lower testosterone
4. Improve Sleep Quality 🛌
Testosterone is primarily produced during deep sleep, especially in the early morning hours. To support hormonal health:
- Aim for 7–8 hours of uninterrupted sleep
- Maintain a consistent sleep schedule
- Avoid blue light and stimulants before bed
- Treat sleep apnea if present
Poor sleep is one of the most overlooked causes of low testosterone and fertility issues.
5. Manage Stress Effectively 😌
Chronic stress leads to elevated cortisol, which suppresses the HPG axis and reduces testosterone. Helpful techniques include:
- Meditation or mindfulness
- Deep breathing exercises
- Nature walks or yoga
- Reducing workload or digital overload
Even 15–30 minutes of daily stress-reducing activity can make a difference.
6. Avoid Environmental Toxins and Endocrine Disruptors ☣️
Limit exposure to chemicals that interfere with hormone production:
- Use glass or stainless steel instead of plastic containers (reduce BPA exposure)
- Choose natural personal care products (free of parabens and phthalates)
- Wash fruits and vegetables to remove pesticide residue
- Avoid smoking and limit alcohol intake
These simple changes help protect the delicate hormonal environment needed for fertility.
7. Consider Natural Supplements (With Medical Advice)
Some supplements have shown promise in supporting male hormonal health:
- Ashwagandha – May increase testosterone and sperm quality
- Fenugreek – May support libido and testosterone levels
- Maca root – Traditionally used to boost sexual health
- L-carnitine – Supports sperm motility
Always consult a healthcare provider before starting supplements, especially if undergoing fertility treatment.
When to Seek Medical Help
While some mild hormonal fluctuations may be temporary or lifestyle-related, persistent symptoms or fertility challenges should not be ignored. Early medical evaluation can help prevent long-term complications and improve the chances of successful treatment.
Key Signs That Require Medical Evaluation
You should see a doctor—preferably a urologist or reproductive endocrinologist—if you experience:
- Low libido or erectile dysfunction lasting more than a few weeks
- Unexplained fatigue, mood changes, or loss of motivation
- Difficulty conceiving after 12 months of regular, unprotected intercourse
- Gynecomastia (breast enlargement) or testicular shrinkage
- Decreased muscle mass or increased body fat without lifestyle changes
- Irregular semen analysis results, especially low sperm count or motility
- Previous or current anabolic steroid use with fertility concerns
- History of pituitary disease, head trauma, or radiation exposure
These symptoms may point to an underlying hormonal imbalance affecting fertility, general health, or both.
Who to See
Depending on your symptoms and goals, the following specialists may be involved:
- Urologist: Specializes in male reproductive health and infertility
- Endocrinologist: Expert in hormonal disorders, including pituitary or thyroid dysfunction
- Reproductive endocrinologist: Specialist in fertility evaluation and treatment
- Andrologist: Focuses specifically on male sexual and reproductive function
Early intervention often leads to better treatment outcomes and may reduce the need for invasive fertility treatments later on.
🔍 What to Expect During Evaluation
- Blood tests to measure hormone levels (testosterone, LH, FSH, prolactin, etc.)
- Semen analysis to assess sperm count and function
- Physical examination of the testes and reproductive system
- Imaging (e.g., pituitary MRI) if clinically indicated
If a hormonal imbalance is confirmed, most men can benefit from targeted therapies, lifestyle adjustments, or fertility-preserving medications.
Frequently Asked Questions (FAQs)
❓ Can low testosterone be reversed naturally?
Yes, in many cases. Mild testosterone deficiency due to lifestyle factors—such as obesity, poor sleep, or stress—can often be reversed through weight loss, exercise, stress management, and better sleep hygiene. However, more severe cases may require medical treatment, especially if there’s a pituitary or testicular disorder.
❓ Is testosterone replacement therapy (TRT) safe for men trying to conceive?
No. While TRT may improve symptoms like low libido or fatigue, it suppresses LH and FSH, leading to a significant drop in sperm production. Men who want to maintain or restore fertility should avoid TRT and consider alternatives like Clomiphene or hCG therapy, which stimulate natural testosterone production without shutting down the HPG axis.
❓ How long does it take to improve fertility after treating hormonal imbalances?
It depends on the cause and severity. In most cases, sperm production begins to improve within 3–6 months of starting appropriate treatment. Full recovery—especially after long-term suppression (e.g., anabolic steroid use)—can take up to 12 months or longer. Periodic semen analysis is used to track progress.
❓ Can high estrogen levels affect male fertility?
Yes. Excess estrogen (estradiol) can suppress the brain’s release of GnRH, which reduces LH and FSH levels—leading to lower testosterone and impaired sperm production. High estrogen is commonly seen in obesity, liver dysfunction, and excess aromatase activity. Treatment may include weight loss, aromatase inhibitors, or managing underlying causes.
❓ Do over-the-counter testosterone boosters work?
Most “testosterone boosters” lack strong clinical evidence and are not regulated. Some herbal supplements (e.g., ashwagandha, fenugreek, maca) may offer modest benefits, but they are not a replacement for medical evaluation and targeted treatment. It’s best to consult a healthcare provider before using any supplement, especially if you’re trying to conceive.
Summary & Final Thoughts
Hormonal balance plays a central role in male fertility, governing everything from testosterone production to sperm quality and sexual function. Disruptions in this delicate system—whether due to lifestyle, medical conditions, or environmental factors—can silently impair reproductive potential.
The good news is that most hormonal imbalances are treatable, and in many cases, reversible. Through proper diagnosis, evidence-based treatment, and supportive lifestyle changes, many men can restore normal hormone levels and significantly improve their fertility outcomes.
If you’re experiencing symptoms such as low libido, fatigue, infertility, or changes in physical health, don’t ignore them. Early testing and medical support can make a real difference—not just in reproductive health, but in your energy, mood, and long-term well-being.
Your fertility is not just a number—it’s a reflection of your overall health. Take care of your hormones, and your body will take care of the rest.