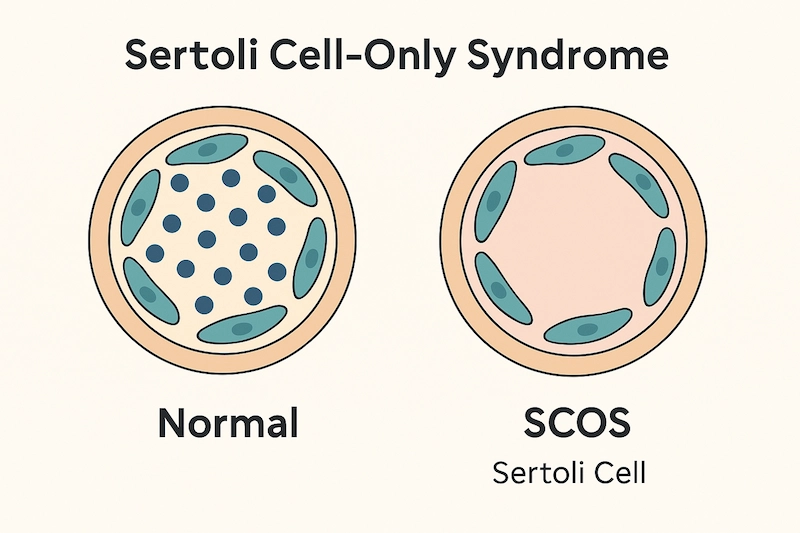
Sertoli Cell-Only Syndrome (SCOS), also known as Del Castillo Syndrome, is a rare condition in which the seminiferous tubules inside the testes contain only Sertoli cells—without the presence of germ cells that develop into sperm. As a result, men with SCOS typically suffer from non-obstructive azoospermia, meaning no sperm is found in the ejaculate due to failed sperm production, not a physical blockage.
Despite being a major cause of male infertility, SCOS often goes undiagnosed until a semen analysis reveals azoospermia. Understanding this condition is essential for accurate diagnosis, realistic expectations about fertility, and identifying potential treatment or family-building options.
In this article, we’ll explore the causes, symptoms, diagnostic process, and the limited—but evolving—treatment options available for men with Sertoli Cell-Only Syndrome.
What Is Sertoli Cell-Only Syndrome?
Sertoli Cell-Only Syndrome (SCOS), also known as Del Castillo Syndrome, is a rare condition in which the seminiferous tubules of the testes contain only Sertoli cells—the supportive cells that help nurture developing sperm cells. However, in SCOS, the germ cells that normally give rise to sperm are entirely absent or extremely scarce, resulting in non-obstructive azoospermia (no sperm in the ejaculate).
The Role of Sertoli Cells in Fertility
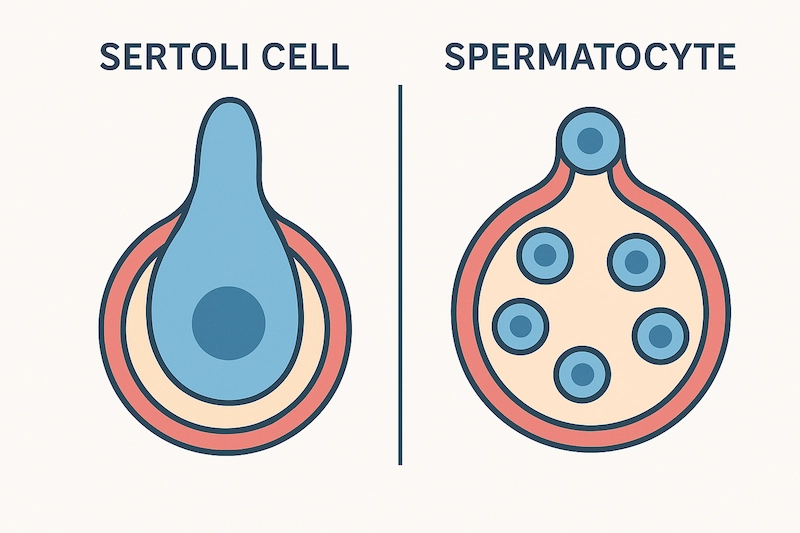
Sertoli cells are essential components of the testes. They:
- Form the blood-testis barrier, which protects developing sperm
- Secrete growth factors and nutrients to support spermatogenesis
- Respond to FSH (follicle-stimulating hormone) from the pituitary
- Coordinate with Leydig cells, which produce testosterone
In healthy testes, Sertoli cells work in conjunction with germ cells (spermatogonia → spermatocytes → spermatids → spermatozoa). In SCOS, this entire germ cell lineage is missing, so no sperm production occurs.
How It Affects Sperm Production
Because SCOS eliminates the source of sperm cells entirely, men with this condition:
- Have no sperm present in the semen (azoospermia)
- Cannot conceive naturally unless viable sperm are found through surgical extraction (which is rare)
- Often have normal male physical development, since Leydig cells still produce testosterone
In rare cases, SCOS may be focal or partial, meaning that a few areas of the testicle may still contain germ cells. In these cases, sperm retrieval via micro-TESE may be possible.
📊 How Common Is It?
- SCOS accounts for approximately 10–20% of cases of non-obstructive azoospermia
- Many men are only diagnosed after attempting to conceive and undergoing fertility testing
- It can be congenital (present from birth) or acquired later in life due to damage from toxins, trauma, or medical treatments
Causes and Risk Factors
Sertoli Cell-Only Syndrome (SCOS) may be congenital (present at birth) or acquired later in life due to damage to the testes. In most cases, the exact cause is unknown, but several risk factors and underlying mechanisms have been identified.
1. Genetic Causes
Genetic abnormalities are among the most well-documented contributors to SCOS. These include:
Y chromosome microdeletions (especially in the AZFa and AZFb regions):
These deletions disrupt genes essential for sperm production.AZFa deletion is strongly associated with SCOS and typically results in complete absence of germ cells.
AZFc deletion, by contrast, may still allow for some residual sperm production.
Klinefelter Syndrome (47,XXY):
Men with an extra X chromosome often develop SCOS due to progressive testicular degeneration starting in puberty.Other chromosomal abnormalities or single-gene mutations may also impair germ cell development.
2. Environmental and Toxic Exposures
Certain external factors can damage the germinal epithelium of the testes and result in acquired SCOS:
- Chemotherapy and radiation therapy – Common in cancer treatment; highly toxic to rapidly dividing germ cells
- Prolonged exposure to toxins – Pesticides, industrial chemicals, heavy metals
- Heat exposure – Repeated high scrotal temperatures (e.g., from undescended testes or frequent sauna use) may contribute over time
- Hormonal disruptors – Long-term exposure to exogenous estrogens or anabolic steroids may impair testicular function
3. Congenital and Developmental Abnormalities
- Cryptorchidism (undescended testicles):
Men with untreated or late-treated undescended testes are at increased risk of SCOS due to temperature-induced germ cell loss. - Testicular dysgenesis syndrome:
A broader term that includes various developmental abnormalities affecting testis formation and function.
4. Varicocele (Possibly Associated)
Some studies suggest a link between large varicoceles and testicular tissue damage that may lead to patterns resembling SCOS. However, this relationship remains controversial, and varicocele is not a definitive cause of SCOS.
🔍 5. Idiopathic Cases (Unknown Origin)
In many men diagnosed with SCOS, no clear cause is found despite thorough evaluation. These idiopathic cases may result from subtle or unidentified genetic or environmental insults occurring early in life.
Symptoms and Clinical Presentation
Sertoli Cell-Only Syndrome (SCOS) often goes unnoticed until fertility testing reveals a problem, because most men with this condition have normal male development and no obvious symptoms. However, there are certain clinical features that may raise suspicion of SCOS—particularly when combined with azoospermia on semen analysis.
❌ 1. Infertility and Azoospermia
The most common and often only noticeable symptom of SCOS is male infertility:
- Men are typically diagnosed after failing to conceive despite regular, unprotected intercourse for 12 months or longer
- Semen analysis shows azoospermia (no sperm in the ejaculate)
- Further investigation is required to determine if the azoospermia is obstructive or non-obstructive
In SCOS, azoospermia is non-obstructive, meaning it results from failed sperm production—not from a physical blockage.
⚖️ 2. Normal Sexual Characteristics
Most men with SCOS have normal testosterone levels (at least initially), which allows for:
- Normal male secondary sexual characteristics (facial/body hair, deep voice)
- Normal libido and erectile function
- Normal muscle mass and fat distribution
This is because Leydig cells (which produce testosterone) are typically unaffected in SCOS.
⚠️ 3. Small or Soft Testicles
Some men may have:
- Smaller-than-average testicular volume
- Soft consistency on palpation (a sign of underactive seminiferous tubules)
However, testicular size alone is not a definitive indicator, and physical examination must be supported by lab tests and imaging.
📉 4. Hormonal Irregularities (in some cases)
While many men have normal hormone levels, some may exhibit:
- Elevated FSH levels – A common finding due to lack of feedback inhibition from germ cells
- Normal or mildly low testosterone – Especially if SCOS is accompanied by testicular damage
- Normal LH – Unless broader testicular dysfunction is present
These findings help distinguish SCOS from other causes of infertility.
Diagnosis and Testing
Diagnosing Sertoli Cell-Only Syndrome (SCOS) requires a combination of clinical evaluation, hormone testing, genetic analysis, and ultimately testicular biopsy. Because SCOS often presents silently—with normal sexual function but no sperm in the semen—diagnosis typically begins during infertility workups.
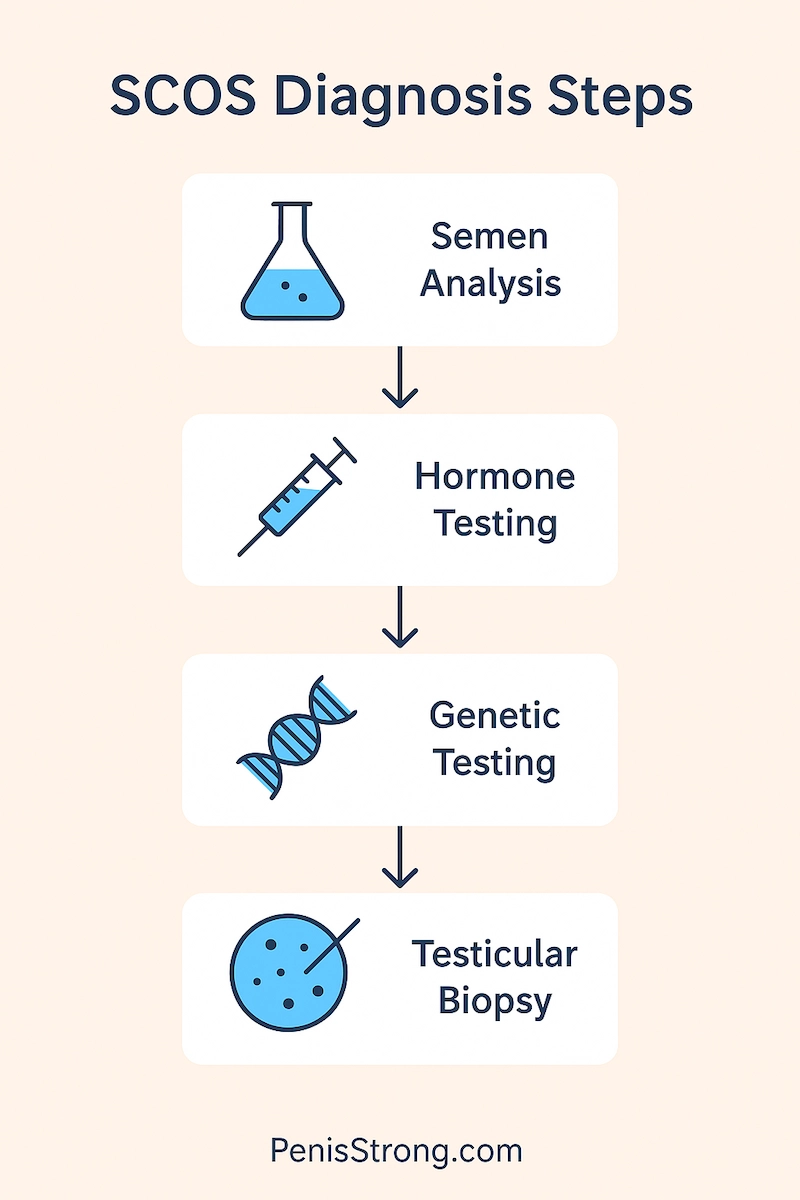
1. Semen Analysis
A standard semen analysis is usually the first step:
Findings:
Azoospermia (no sperm in the ejaculate)
Normal semen volume, pH, and liquefaction in most cases
Requires at least two separate tests, spaced weeks apart, to confirm azoospermia
Semen analysis alone cannot confirm SCOS but raises suspicion for non-obstructive azoospermia.
2. Hormonal Testing
Blood tests help differentiate primary testicular failure from hypothalamic or pituitary causes (secondary hypogonadism):
| Hormone | Typical Finding in SCOS |
|---|---|
| FSH | Elevated (common) |
| LH | Normal or mildly high |
| Testosterone | Normal or slightly low |
| Inhibin B | Often low or undetectable (reflects Sertoli cell dysfunction) |
High FSH is a hallmark feature, indicating poor feedback from the damaged seminiferous tubules.
3. Genetic Testing
Recommended for all men with non-obstructive azoospermia to rule out underlying chromosomal abnormalities:
- Karyotype analysis – To detect Klinefelter syndrome (47,XXY) or other chromosomal defects
- Y chromosome microdeletion testing – Focused on AZF regions
AZFa or AZFb deletions strongly suggest complete SCOS and predict poor prognosis for sperm retrieval
Genetic findings also guide family planning and determine the feasibility of assisted reproduction.
4. Scrotal Ultrasound
Scrotal ultrasound can assess:
- Testicular volume and consistency
- Presence of varicocele, masses, or structural abnormalities
- May support the diagnosis but cannot confirm SCOS alone
Ultrasound is non-invasive and helpful in evaluating associated findings.
5. Testicular Biopsy (Definitive Diagnosis)
A testicular biopsy is the gold standard for diagnosing SCOS. It involves extracting a small tissue sample from the testicle and examining it under a microscope.
Histological findings in SCOS:
Seminiferous tubules lined exclusively by Sertoli cells
Absence of germ cells (no spermatogonia or spermatocytes)
In rare focal SCOS, some regions may contain germ cells—allowing potential for sperm retrieval
Biopsy may be performed during diagnostic workup or sperm retrieval procedures such as micro-TESE.
Treatment Options for SCOS
There is currently no cure for Sertoli Cell-Only Syndrome (SCOS), as the condition involves the complete or near-complete absence of germ cells, which are necessary for sperm production. However, depending on whether the condition is complete or focal (partial), there may be limited options for achieving biological fatherhood, as well as ways to manage hormonal symptoms and support emotional well-being.
1. Is SCOS Reversible?
Unfortunately, SCOS is not reversible in most cases. Once germ cells are absent from the seminiferous tubules, they cannot regenerate spontaneously. However, some men may have focal SCOS, where small areas of the testicle still produce sperm.
These cases may allow for:
- Surgical sperm retrieval using advanced microsurgical techniques
- Attempted biological fatherhood via ICSI (intracytoplasmic sperm injection)
🔍 2. Micro-TESE (Microsurgical Testicular Sperm Extraction)
Micro-TESE is the most effective method for attempting sperm retrieval in SCOS patients. It involves:
- A surgical procedure under a microscope to locate rare areas of sperm production
- Tissue samples are examined for viable sperm, which can be frozen or used immediately for IVF-ICSI
Success rate is typically low in SCOS (around 10–30%), but it offers a chance of biological paternity in focal cases.
📝 Note: Men with complete SCOS and AZFa deletions are not candidates for micro-TESE, as these cases predict complete absence of germ cells.
3. Hormonal Therapy (for Symptom Management)
While hormone therapy does not restore sperm production, it may help men with:
- Low testosterone symptoms (fatigue, low libido, muscle loss)
- Mood changes or osteopenia related to hypogonadism
Treatment options include:
- Testosterone replacement therapy (TRT)
- Monitoring of FSH, LH, and estradiol to maintain hormonal balance
⚠️ Caution: TRT will suppress any residual sperm production, so it should be considered only after fertility preservation attempts are completed.
4. Assisted Reproductive Technologies (ART)
If sperm is successfully retrieved via micro-TESE, conception is only possible through ICSI, which involves:
- Injecting a single viable sperm directly into the egg during IVF
- Often combined with genetic screening of embryos, especially if genetic mutations are present in the male partner
In the majority of SCOS cases where no sperm is found, couples must explore alternative family-building options.
5. Use of Donor Sperm
When no sperm can be retrieved, or if the couple chooses to avoid surgical options, donor sperm offers a safe and effective alternative:
- Can be used with IUI (intrauterine insemination) or IVF
- Requires psychological counseling and informed consent
- High success rates, especially when the female partner has no fertility issues
While it does not allow for biological fatherhood, this option enables many men with SCOS to become parents.
Emotional and Psychological Support
A diagnosis of Sertoli Cell-Only Syndrome can be emotionally devastating. For many men, fertility is closely tied to identity, masculinity, and future family plans. Learning that natural conception may be impossible—or that sperm may be entirely absent—can lead to a deep emotional impact that affects not only the individual, but also the relationship.
1. Coping with a Diagnosis of Male Infertility
Men with SCOS often experience:
- Shock or disbelief upon hearing that no sperm are present
- Guilt or shame, especially in cultures where fertility is strongly valued
- Grief, similar to mourning the loss of a biological child
- Anger, frustration, or sadness, particularly if the cause is genetic or unavoidable
These emotions are completely valid. Recognizing them is the first step toward healing.
2. Counseling and Support Groups
Mental health support is just as important as medical treatment. Helpful resources include:
- Individual counseling – With a therapist familiar with infertility and men’s health
- Couples therapy – To navigate decisions about ART, donor sperm, or adoption
- Support groups – Online or local communities of men or couples facing similar challenges
Talking openly can reduce feelings of isolation and help normalize the experience.
3. Communicating with a Partner
Infertility can create strain in even the strongest relationships. Open, honest, and empathetic communication is essential:
- Share emotional reactions and fears
- Make decisions together about testing and treatment
- Be patient with each other’s pace of acceptance
It’s a shared journey—not a solo struggle.
📌 4. Making Peace with the Outcome
Whether or not a biological child is possible, many men find meaning and joy through:
Donor conception
Adoption
Mentorship, family roles, or community involvement
There is no “one way” to be a father or to build a family.
Outlook and Fertility Alternatives
Sertoli Cell-Only Syndrome (SCOS) presents a significant challenge to male fertility, but it does not mean the end of fatherhood. With the help of modern reproductive technologies, supportive counseling, and alternative parenting paths, many men with SCOS go on to build fulfilling families and lead emotionally healthy lives.
1. Prognosis for Biological Fatherhood
The chance of fathering a biological child depends on whether focal areas of spermatogenesis are present:
- Men with complete SCOS (confirmed by AZFa deletion or biopsy) typically cannot produce sperm, even with advanced techniques
- Those with focal SCOS may have small areas in the testes that produce sperm—making micro-TESE + ICSI a possible option
- Success rates for sperm retrieval in SCOS are low (10–30%), but not zero
Genetic testing results are critical in predicting these outcomes and guiding decisions.
2. Importance of Early Evaluation
Men who are diagnosed with SCOS at a younger age—particularly before undergoing treatments like chemotherapy or radiation—should explore:
- Sperm cryopreservation if any sperm is found
- Early fertility counseling with a reproductive urologist
- Genetic counseling for long-term reproductive planning
Time-sensitive evaluation can expand future options.
3. Donor Sperm as a Viable Alternative
When sperm cannot be retrieved, donor insemination offers a highly effective path to parenthood:
- Often combined with intrauterine insemination (IUI) or IVF
- Allows the female partner to carry and deliver the child
- Requires legal and emotional preparation, often including counseling
Many couples report deep emotional bonding and fulfillment with donor-conceived children.
4. Adoption and Other Family-Building Options
Adoption is another meaningful way to become a parent, offering:
- The opportunity to provide a loving home to a child in need
- Fulfillment of parenting goals outside the biological path
- A long-standing, widely accepted alternative for SCOS families
Every path is valid—and personal.
📌 Key Takeaway:
While SCOS presents permanent limitations in most cases, it does not prevent men from becoming fathers or building families. With the right support and planning, there are multiple fulfilling options—biological or not.
Frequently Asked Questions (FAQs)
❓ Can Sertoli Cell-Only Syndrome be cured?
No. SCOS is considered irreversible in most cases because the germ cells necessary for sperm production are absent. However, some men may have focal areas with limited sperm production that allow for retrieval through micro-TESE.
❓ Is it possible to father a biological child with SCOS?
It depends. Men with focal SCOS may be able to retrieve sperm through micro-TESE and use it with ICSI for conception. However, for those with complete SCOS (especially with AZFa deletion), biological fatherhood is not possible.
❓ Does SCOS affect testosterone or sexual function?
In many cases, testosterone levels and sexual function remain normal, as Leydig cells are not affected. However, some men may develop low testosterone over time and benefit from hormone therapy.
❓ What are the treatment options if no sperm is found?
If sperm retrieval is unsuccessful, couples can explore:
- Donor sperm insemination (IUI/IVF)
- Adoption
- Emotional and psychological counseling to support the decision-making process
❓ Should all men with SCOS get genetic testing?
Yes. Karyotype analysis and Y chromosome microdeletion testing are strongly recommended to identify genetic causes, determine prognosis, and guide reproductive planning—especially if ART is considered.
Summary & Final Thoughts
Sertoli Cell-Only Syndrome (SCOS) is a rare but serious condition that causes non-obstructive azoospermia due to the absence of germ cells in the testes. While the diagnosis often comes as a shock—especially to men who otherwise appear healthy and have no symptoms—it is important to remember that infertility does not define a man’s identity, worth, or future as a parent.
Although SCOS is generally irreversible, focal cases may still offer a chance for biological fatherhood through advanced sperm retrieval techniques and assisted reproduction. For those without this option, donor sperm, adoption, and other family-building paths provide meaningful, fulfilling alternatives.
Most importantly, men with SCOS are not alone. With the right combination of medical care, emotional support, and open communication, it is absolutely possible to move forward with confidence, clarity, and hope.
If you or your partner are navigating a diagnosis of SCOS, don’t hesitate to reach out to a fertility specialist and connect with others who have walked a similar path. Your journey is valid—and so is your future.