Sexually transmitted infections (STIs), also known as sexually transmitted diseases (STDs), are infections passed from one person to another through sexual contact. They can be caused by bacteria, viruses, or parasites and may affect various parts of the body—including the genitals, mouth, and rectum.
STIs are more common than many people think, and some can remain asymptomatic, meaning they spread easily without showing signs. When left untreated, they can lead to serious complications, such as infertility, chronic pain, or increased risk of HIV.
This overview will help you understand the types of STIs, how they are transmitted, common symptoms, and most importantly—how to protect yourself and your partners.
What Are Sexually Transmitted Infections (STIs)?
Sexually transmitted infections (STIs), also called sexually transmitted diseases (STDs), are infections passed primarily through sexual contact. This includes vaginal, oral, and anal sex, as well as intimate skin-to-skin contact in some cases.
While the term STD is still commonly used, STI is now more widely accepted in the medical community because:
- Not all infections cause obvious disease or symptoms
- Many people carry infections without knowing, but can still transmit them
What Causes STIs?
STIs are caused by a range of microorganisms:
- Bacteria (e.g., Chlamydia, Gonorrhea, Syphilis)
- Viruses (e.g., HIV, Herpes simplex virus (HSV), HPV)
- Parasites (e.g., Trichomonas vaginalis, pubic lice)
These organisms thrive in moist environments like the genitals, rectum, and throat, and can be easily transferred between partners.
👨⚕️ Why Are STIs Important to Understand?
STIs are more common than many people realize. Millions of new cases occur every year worldwide—and many go undetected because they cause no immediate symptoms.
Understanding STIs is crucial because:
- They can lead to serious complications if untreated (e.g., infertility, chronic pain, cancer, HIV transmission)
- Most are treatable or manageable with proper care
- Testing is easy, fast, and often confidential

How Do STIs Spread?
Sexually transmitted infections (STIs) are primarily spread through sexual and intimate contact, but the exact mode of transmission depends on the specific infection. Understanding how STIs are passed from person to person is key to prevention.
1. Vaginal, Oral, and Anal Sex
Most STIs are transmitted through direct contact with infected bodily fluids, including semen, vaginal fluids, and blood. This can happen during:
- Vaginal intercourse
- Anal sex (higher risk for tearing and blood exposure)
- Oral sex (especially for herpes, gonorrhea, syphilis, HPV)
Even without ejaculation, the virus or bacteria can still spread through skin contact or pre-ejaculate fluid.
2. Skin-to-Skin Contact
Some STIs, such as herpes (HSV) and HPV, can spread through contact with infected skin or mucous membranes, even when no fluids are exchanged. This means:
- Condoms may reduce but not eliminate the risk
- Sores or warts outside the condom-covered area can still transmit infection
3. Sharing Needles or Injection Equipment
STIs such as HIV and hepatitis B/C can be transmitted through:
- Sharing needles for drug use
- Contaminated tattoo or piercing tools
- Medical instruments that are not properly sterilized
4. Mother-to-Child Transmission
Some STIs can pass from an infected mother to her baby:
- During pregnancy (e.g., syphilis, HIV)
- During childbirth (e.g., gonorrhea, herpes)
- Through breastfeeding (e.g., HIV)
Proper prenatal care and treatment can greatly reduce these risks.
❗ Important Notes:
- Asymptomatic individuals can still spread STIs
- Some infections can be spread even when using condoms, especially those transmitted via skin contact
- Mutual monogamy and regular testing are among the most effective ways to reduce risk
Common Types of STIs in Men
STIs in men can be caused by bacteria, viruses, or parasites, each with its own set of symptoms, complications, and treatment options. Below is an overview of the most common STIs that affect men.
Bacterial STIs
These are typically curable with antibiotics if diagnosed early.
- Chlamydia: Often silent; may cause burning urination, discharge, or testicular pain
- Gonorrhea: Similar to chlamydia but often more symptomatic; can cause complications in the urethra and testicles
- Syphilis: Presents in stages; starts with painless sores, progresses to rash and neurological symptoms if untreated
Viral STIs
These are not curable, but can be managed with medication and proper care.
- Herpes Simplex Virus (HSV): Causes painful blisters or sores on the genitals or mouth; can recur
- Human Papillomavirus (HPV): Some strains cause genital warts; others linked to penile and throat cancer
- HIV (Human Immunodeficiency Virus): Attacks the immune system; can lead to AIDS if untreated
- Hepatitis B and C: Affect the liver; can be transmitted sexually or through blood
Parasitic STIs
Generally curable but often underdiagnosed.
- Trichomoniasis: May cause itching, discharge, or burning after urination
- Pubic lice (crabs): Tiny parasites that live in pubic hair and cause intense itching
- Scabies: Mites that burrow into the skin, causing rash and irritation
📌 Each of these infections will be explored in more detail in separate articles. Knowing their names and general effects helps you recognize when something might be wrong—and when to get tested.
Signs and Symptoms of STIs in Men
Sexually transmitted infections (STIs) don’t always announce themselves with obvious symptoms—many men have no idea they’re infected. However, when symptoms do appear, they often affect the genital area, urinary system, or skin.
⚠️ Common Symptoms to Watch For:
1. Painful or Burning Urination
A common sign of bacterial STIs like chlamydia or gonorrhea.
2. Discharge from the Penis
Yellow, green, or white discharge from the urethra may signal infection.
3. Genital Sores, Blisters, or Ulcers
Painful sores = often herpes (HSV)
Painless sores = may be syphilis (primary stage)
4. Itching, Redness, or Irritation
Common with trichomoniasis, pubic lice, or scabies.
5. Pain or Swelling in the Testicles
Can be a complication of chlamydia or gonorrhea if the infection spreads.
6. Genital Warts
Caused by HPV; may appear as small, flesh-colored bumps or clusters.
7. Rash on the Body, Palms, or Soles
Often seen in secondary syphilis.
8. Rectal Symptoms (if receptive anal sex)
Pain, bleeding, or discharge from the rectum can indicate infection.
Asymptomatic Infections
Many STIs—especially chlamydia, HPV, and HIV in early stages—can show no symptoms at all. You or your partner may carry and spread the infection unknowingly.
📍 Regular testing is the only reliable way to know your status—even if you feel completely fine.
Potential Complications if Left Untreated
Sexually transmitted infections (STIs) aren’t just a short-term inconvenience—they can lead to serious, long-lasting health problems when ignored or untreated. Even infections that seem minor or cause no symptoms can quietly cause damage over time.
1. Epididymitis and Infertility
Untreated chlamydia and gonorrhea can spread to the epididymis (a tube near the testicles), causing pain, swelling, and potentially permanent infertility if scarring occurs.
2. Chronic Pelvic or Testicular Pain
Persistent infection or inflammation can lead to ongoing discomfort or pain, even after the infection is cleared.
3. Penile Disfigurement or Sores
- Syphilis can progress to large, ulcerated lesions or internal organ damage
- HPV can cause persistent genital warts or, in rare cases, penile cancer
4. Increased Risk of HIV
Having an untreated STI (especially one that causes sores or inflammation like herpes or syphilis) significantly increases your risk of contracting or transmitting HIV.
5. Long-Term Organ and Immune System Damage
- Untreated HIV weakens the immune system and can lead to AIDS
- Late-stage syphilis can damage the brain, heart, and nerves
6. Transmission to Others
You may unknowingly pass the infection to:
- Sexual partners
- A future long-term partner
- In rare cases, newborns, if the infection is passed from mother during delivery
📍 The bottom line: STIs are often easy to treat—but ignoring them can cause permanent harm to you and others.
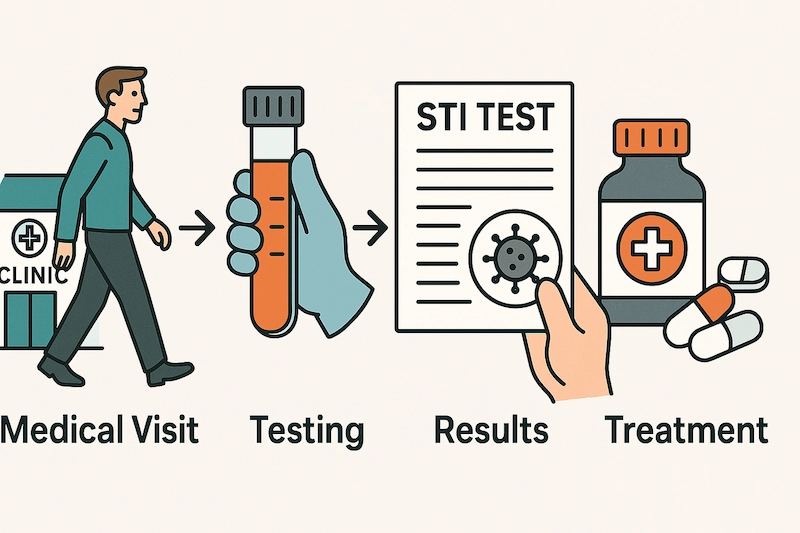
STI Testing and Diagnosis
Getting tested for STIs is one of the most responsible steps you can take to protect your sexual health—and your partners. Testing is quick, confidential, and widely available, and many infections can be treated effectively if caught early.
🔍 1. When Should You Get Tested?
You should consider testing if you:
- Have had unprotected sex with a new partner
- Have multiple partners
- Show any symptoms (e.g., discharge, pain, sores)
- Know or suspect that a partner has an STI
- Are starting a new relationship and want to test together
- Are a man who has sex with men (MSM)
- Have previously been diagnosed with an STI
👉 Even if you have no symptoms, regular screening is recommended every 6–12 months if you’re sexually active with multiple partners.
2. How Are STIs Diagnosed?
Diagnosis usually involves a combination of the following tests:
- Urine samples – for chlamydia, gonorrhea
- Blood tests – for HIV, syphilis, hepatitis B/C, HSV
- Swab tests – from the urethra, throat, or rectum
- Physical examination – to check for visible symptoms (warts, sores, discharge)
Most tests are fast, painless, and can be done at a clinic or with a home test kit.
3. Is STI Testing Confidential?
Yes. STI testing is confidential in most countries. Clinics and providers will not share your results with anyone without your consent. In many places, anonymous or low-cost testing is available.
🧭 4. What If You Test Positive?
- Don’t panic—most STIs are treatable, and many are curable
- Your healthcare provider will explain the next steps
- You may be advised to inform partners so they can get tested
- Treatment is usually straightforward and highly effective
📍 Testing is not about judgment—it’s about knowing your status, staying healthy, and showing care for yourself and your partners.
Prevention Strategies
While no method is 100% foolproof (aside from abstinence), there are several highly effective strategies men can use to reduce the risk of contracting or spreading STIs. Prevention is not just about protection—it’s about awareness, responsibility, and communication.
✅ 1. Use Condoms Correctly and Consistently
Condoms are one of the most effective tools in STI prevention when used properly.
- Use latex or polyurethane condoms for vaginal, anal, and oral sex
- Put on a new condom before any genital contact
- Never reuse condoms
- Consider dental dams for oral sex on the anus or vulva
📍 Condoms greatly reduce the risk of HIV, chlamydia, gonorrhea, and more—but may offer less protection for skin-to-skin STIs like herpes or HPV.
✅ 2. Get Tested Regularly
Regular STI screening helps detect infections before symptoms appear. Early detection protects both you and your partners.
- Every 6–12 months for sexually active individuals
- Before new sexual relationships
- Immediately if symptoms appear or exposure is suspected
✅ 3. Get Vaccinated
Some STIs are preventable with vaccines:
- HPV vaccine: Protects against strains causing genital warts and cancers
- Hepatitis B vaccine: Offers long-term protection against liver infection
📍 Vaccination is especially important if you’re under 26 or at higher risk.
✅ 4. Limit Number of Sexual Partners
Reducing the number of sexual partners lowers your overall risk. If you’re in a monogamous relationship, make sure both partners are tested and clear.
✅ 5. Talk Openly with Partners
Having honest conversations about STI history, testing, and protection can help:
- Build trust
- Prevent misunderstandings
- Encourage safer choices
Don’t assume—ask and share your status honestly.
✅ 6. Avoid Sharing Needles or Personal Items
Sharing needles for drug use or even personal grooming tools (like razors) increases risk for HIV, hepatitis B and C.
📍 Prevention is about progress, not perfection. Using a combination of these strategies gives you the best protection—and peace of mind.
Treatment and Management
The good news is that most STIs are treatable, and many are curable, especially when detected early. With the right medical care, you can manage or eliminate the infection—and prevent spreading it to others.
1. Antibiotic Treatment (for Bacterial STIs)
STIs caused by bacteria are typically curable with prescribed antibiotics.
- Chlamydia, gonorrhea, and syphilis can often be cured with a single dose or short course of antibiotics
- It’s crucial to complete the full course, even if symptoms disappear
- Avoid sex until your doctor confirms the infection is cleared
2. Antiviral Medications (for Viral STIs)
While viral infections like herpes (HSV) and HIV can’t be cured, they can be effectively managed with daily antiviral therapy.
- Herpes: Antivirals like acyclovir or valacyclovir help reduce outbreaks and transmission
- HIV: Antiretroviral therapy (ART) lowers viral load to undetectable = untransmittable (U=U)
- HPV: No cure, but warts can be treated and most infections clear on their own over time
3. Partner Notification and Treatment
If you test positive for an STI, it’s important to inform your current and recent sexual partners so they can get tested and treated. Some clinics offer anonymous partner notification services.
4. Avoid Re-Infection
- Refrain from sex until treatment is completed and symptoms resolve
- Use protection consistently moving forward
- Schedule follow-up testing if recommended
5. Emotional and Psychological Support
A positive STI result can bring anxiety, shame, or fear. But remember:
- STIs are common and treatable
- Getting treatment shows courage and responsibility
- Don’t hesitate to seek mental health support if needed
📍 Proper treatment doesn’t just clear the infection—it breaks the chain of transmission and helps you reclaim control over your health.
Reducing Stigma Around STIs
Despite how common sexually transmitted infections (STIs) are, stigma, shame, and misinformation still prevent many people—especially men—from seeking testing, talking to partners, or getting treatment.
Breaking down that stigma is key to better sexual health for everyone.
1. STIs Are Medical Conditions, Not Moral Failures
Having an STI doesn’t mean you’re irresponsible, dirty, or unfaithful. It means you’ve been sexually active—like most adults. STIs are simply infections, and they can happen to anyone, regardless of lifestyle, orientation, or relationship status.
💬 2. Normalize Testing and Conversation
Regular STI testing should be as routine as dental checkups. The more we:
- Talk about it
- Ask about it
- Get tested without shame
…the more we normalize healthy sexual habits.
3. Support Partners with Compassion
If a partner discloses an STI:
- Listen without judgment
- Ask questions respectfully
- Offer support and take shared responsibility for protection and testing
Remember: how we react to STI conversations sets the tone for future trust.
4. Use Accurate Sources of Information
Avoid relying on rumors or outdated ideas. Stick to:
- Verified medical websites
- Trusted health providers
- Reputable clinics and public health organizations
Misinformation fuels stigma. Knowledge fights it.
📍 The more we talk about STIs openly and respectfully, the safer and healthier our communities become. There’s no shame in knowing your status—only power.
FAQs About STIs in Men
❓ Are STIs always noticeable in men?
No. Many STIs have no symptoms, especially in the early stages. You can be infected—and contagious—without knowing it.
❓ Can I get an STI from oral or anal sex?
Yes. STIs can spread through oral, anal, or vaginal sex, and even through skin-to-skin contact with infected areas.
❓ Do condoms protect against all STIs?
Condoms greatly reduce the risk of many STIs (like HIV, chlamydia, gonorrhea), but they don’t fully protect against infections spread through skin contact, such as herpes or HPV.
❓ How often should I get tested?
If you’re sexually active with multiple partners, get tested every 6 to 12 months—or sooner if you notice symptoms or have a new partner.
❓ Can STIs affect fertility?
Yes. Untreated STIs like chlamydia or gonorrhea can lead to infertility by damaging the testicles or reproductive tract.
❓ Is it possible to get the same STI more than once?
Yes. Being treated once doesn’t make you immune. You can be reinfected if you’re exposed again, especially with bacterial STIs.
❓ Do I need to tell my partner if I have an STI?
Yes. It’s important to be honest so your partner can get tested and treated too. Some clinics offer anonymous partner notification services if needed.
Final Thoughts
Sexually transmitted infections (STIs) are far more common—and far more manageable—than most people think. With modern testing, effective treatments, and vaccines, we have more tools than ever to protect our sexual health.
But the first step is knowledge.
Whether you’re experiencing symptoms, entering a new relationship, or simply taking charge of your health, getting tested and staying informed shows responsibility—not weakness. Regular screenings, open conversations, and safe sex practices can protect not only your own well-being but also that of your partners.
👉 Remember: knowing your status isn’t just smart—it’s empowering. STIs are nothing to be ashamed of, and they’re almost always treatable with the right care.