Sperm health plays a crucial role in male fertility, and one of the most important indicators is sperm motility—the ability of sperm to swim efficiently toward the egg. Even if sperm count is normal, poor motility can significantly reduce the chances of natural conception.
Many factors influence sperm motility, including lifestyle habits, hormonal balance, infections, and underlying health conditions. The good news is that in many cases, poor sperm motility can be improved through targeted medical treatment and natural lifestyle changes.
In this comprehensive guide, we’ll explore what sperm motility is, why it matters, how it’s tested, and practical strategies to boost it and support overall sperm health.
What Is Sperm Motility?
Sperm motility refers to the ability of sperm to move efficiently through the female reproductive tract to reach and fertilize the egg. It is one of the most critical aspects of male fertility—without proper motility, sperm may not be able to navigate the cervical mucus, uterus, and fallopian tubes.
Types of Sperm Motility
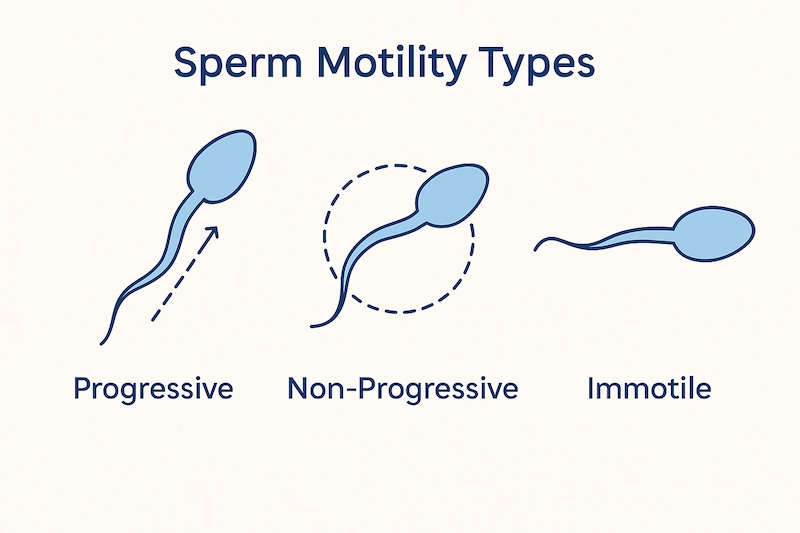
According to the World Health Organization (WHO), sperm motility is categorized into three main types:
Progressive Motility (PR):
Sperm that swim actively in a straight line or large circles—this type is essential for reaching and fertilizing the egg.Non-Progressive Motility (NP):
Sperm that move but do not make forward progress (e.g., swim in tight circles or barely move forward).Immotile (IM):
Sperm that show no movement at all.
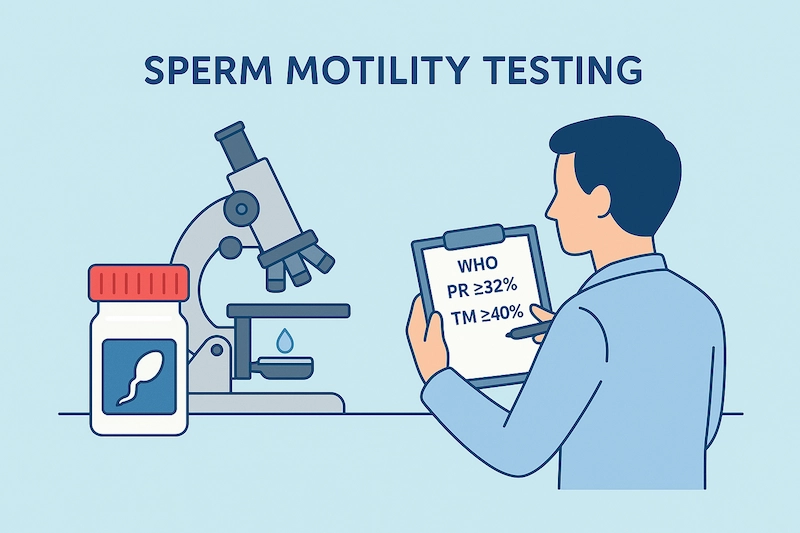
Healthy sperm motility is defined by the percentage of sperm with progressive movement. According to WHO 2010 guidelines:
Normal reference range:
≥ 40% total motile sperm (progressive + non-progressive)
OR
≥ 32% progressively motile sperm
Anything below these thresholds is considered asthenozoospermia—a condition of reduced sperm motility that may impair natural conception.
Why Sperm Motility Matters
Even if sperm count is high, low motility can significantly reduce fertility because the sperm may not reach the egg. Good motility increases the likelihood of:
- Penetrating cervical mucus
- Navigating the female reproductive tract
- Successfully fertilizing the egg
In fact, many couples with unexplained infertility may later discover that sperm motility is the limiting factor in achieving pregnancy.
How Is Sperm Motility Tested?
Sperm motility is assessed through a laboratory procedure called semen analysis, which evaluates multiple aspects of a man’s ejaculate, including sperm count, shape, volume, and movement. This test is a core part of male fertility evaluations and helps determine the likelihood of natural conception.
Semen Analysis (Standard Method)
Semen analysis is typically performed after 2–5 days of sexual abstinence. The sample is collected by masturbation into a sterile container and analyzed within 30–60 minutes to ensure accurate motility assessment.
The lab examines:
- Total motility: Percentage of all sperm that are moving (progressive + non-progressive)
- Progressive motility (PR): Percentage of sperm moving forward effectively
- Non-progressive motility (NP): Sperm with weak or unproductive movement
- Immotile sperm (IM): Sperm showing no movement
WHO 2010 Reference Values:
- Total motility ≥ 40%
- Progressive motility ≥ 32%
Anything below these values suggests impaired motility (asthenozoospermia).
🔬 Motility Grading System
Some labs use a grading system to categorize motility more precisely:
- Grade A (rapid progressive): Strong forward motion, straight line
- Grade B (slow progressive): Forward motion, but slower or less linear
- Grade C (non-progressive): No forward progression despite movement
- Grade D (immotile): Completely stationary sperm
Higher percentages of Grade A and B sperm indicate better fertility potential.
📊 Computer-Assisted Sperm Analysis (CASA)
In some advanced fertility centers, motility is evaluated using CASA (Computer-Assisted Sperm Analysis)—a system that provides precise, objective measurements of:
- Velocity
- Path trajectory
- Sperm tracking over time
CASA improves accuracy and consistency, especially for clinics offering assisted reproductive technologies (ART).
📌 Key Takeaway
Sperm motility is not just about whether sperm are moving—but how efficiently they are moving toward the egg. A semen analysis provides crucial insight into motility status and helps guide further investigation or treatment if needed.
Causes of Poor Sperm Motility (Asthenozoospermia)
Asthenozoospermia is the medical term for reduced sperm motility, and it is one of the leading causes of male infertility. Poor sperm motility can result from a wide range of lifestyle, environmental, medical, and genetic factors—many of which are preventable or treatable.
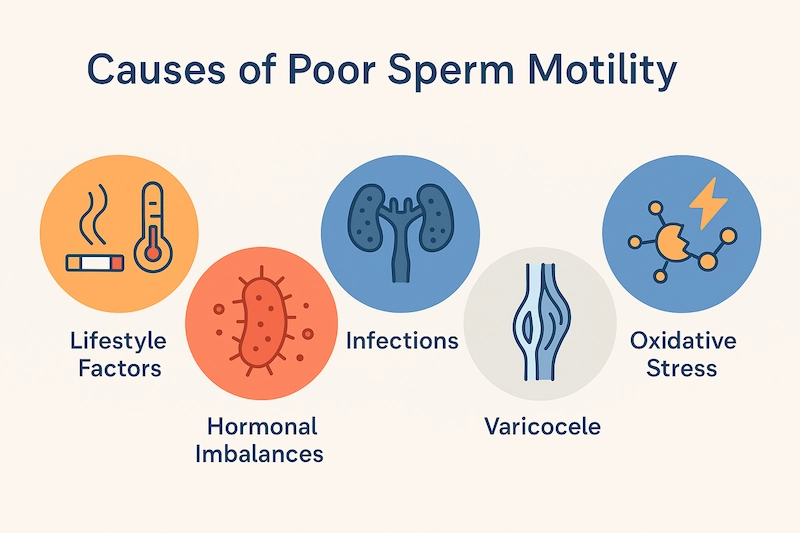
1. Lifestyle Factors
Several everyday habits can negatively affect sperm motility:
- Smoking – Increases oxidative stress, damages sperm DNA, and impairs movement
- Excessive alcohol consumption – Disrupts hormone balance and sperm quality
- Obesity – Associated with hormonal imbalance (low testosterone, high estrogen)
- Sedentary lifestyle – Linked to poor circulation and increased scrotal temperature
- Heat exposure – Frequent use of hot tubs, saunas, or tight underwear raises testicular temperature and affects motility
- Chronic stress – Can alter hormone levels and increase cortisol, impacting sperm production
2. Hormonal Imbalances
Testosterone and other reproductive hormones play a key role in sperm development and motility. Conditions that reduce hormone levels include:
- Hypogonadism (low testosterone)
- Thyroid dysfunction (hypo- or hyperthyroidism)
- High prolactin levels
- Insulin resistance and metabolic syndrome
These conditions may impair both sperm production and quality.
3. Infections
Certain infections can affect the prostate, seminal vesicles, or testes and disrupt the environment necessary for healthy sperm motility:
- Sexually transmitted infections (e.g., chlamydia, gonorrhea)
- Prostatitis
- Epididymitis or orchitis
- Systemic infections with fever (temporary motility decline)
Prompt diagnosis and antibiotic treatment are essential.
4. Varicocele
A varicocele is an enlargement of the veins within the scrotum, which increases testicular temperature and reduces oxygen supply. This condition:
- Causes oxidative stress
- Impairs sperm production
- Is found in up to 40% of men with abnormal semen parameters
Surgical correction (varicocelectomy) often improves motility.
5. Oxidative Stress and DNA Damage
Reactive oxygen species (ROS) can damage sperm membranes and impair their ability to move effectively. Causes include:
- Smoking
- Environmental toxins
- Poor diet
- Excessive exercise or stress
Antioxidants such as vitamin C, E, CoQ10, and zinc may help counteract this effect.
6. Genetic or Structural Abnormalities
In rare cases, low motility may be linked to:
- Genetic defects in flagellar proteins
- Ciliary dyskinesia (e.g., Kartagener syndrome)
- Structural abnormalities of the tail or midpiece of the sperm
These conditions are often diagnosed through specialized testing and may not be reversible.
📌 Key Insight:
Because poor sperm motility may have multiple overlapping causes, a comprehensive evaluation—including lifestyle review, hormonal testing, and semen analysis—is essential to guide treatment.
Other Key Factors of Sperm Health
While sperm motility is a critical factor in male fertility, it’s only one part of the bigger picture. A healthy sperm must also have the right number, structure, and vitality to successfully fertilize an egg. Semen analysis evaluates several additional parameters to assess overall sperm health.
1. Sperm Count (Concentration)
This refers to the number of sperm cells present in a milliliter of semen.
- Normal range (WHO 2010): ≥15 million sperm/mL
- A low sperm count (oligospermia) can reduce the chances of fertilization, especially if motility or morphology is also poor.
- Azoospermia refers to the complete absence of sperm in the semen.
Sperm motility and count often go hand in hand, but not always.
2. Sperm Morphology (Shape)
Sperm should have a normal oval-shaped head, a midpiece, and a long tail to swim efficiently. Abnormal shapes can affect:
- The sperm’s ability to penetrate the egg
- Motility and direction of movement
WHO considers ≥4% of normally shaped sperm (using strict Kruger criteria) as acceptable. Higher percentages indicate better fertility potential.
3. Semen Volume and pH
- Normal semen volume: 1.5–6.0 mL
- Low volume may indicate issues with seminal vesicles or ejaculatory ducts
- pH range: 7.2–8.0
Too acidic or alkaline environments can harm sperm motility and survival
4. Sperm Vitality (Live vs. Dead Sperm)
Motility only assesses moving sperm, but not all immotile sperm are dead. Vitality testing determines the percentage of live sperm, even if they’re not motile.
- A normal vitality result is ≥58% live sperm
- Low vitality combined with poor motility suggests severe damage or degeneration
5. Sperm DNA Integrity
While not routinely tested, DNA fragmentation can impair fertilization, embryo development, and increase miscarriage risk. Causes include:
- Oxidative stress
- Smoking
- Age
- Environmental toxins
Specialized tests (e.g., SCSA, TUNEL, COMET) can assess DNA quality.
📌 Bottom Line:
Fertility specialists look at the full picture of sperm health—not just motility. Combining good motility with healthy count, shape, and vitality gives the best chance of natural or assisted conception.
Medical Treatments for Low Sperm Motility
The treatment for poor sperm motility depends on the underlying cause, the severity of the motility defect, and the couple’s fertility goals. In many cases, addressing the root cause and making targeted medical interventions can improve sperm motility and enhance the chances of conception—either naturally or with assisted reproductive technologies (ART).
1. Treating Infections
If a bacterial infection such as prostatitis, epididymitis, or a sexually transmitted infection (STI) is impairing sperm motility, treatment with appropriate antibiotics or anti-inflammatory medications may improve sperm function.
- It’s important to treat both partners if an STI is involved
- A follow-up semen analysis is usually performed after treatment
2. Hormonal Therapy
If poor motility is due to hormonal imbalance (e.g., low testosterone, elevated prolactin, thyroid issues), hormone levels can often be corrected using:
- Clomiphene citrate (Clomid) – Stimulates the brain to produce more LH and FSH, boosting testosterone and sperm production
- hCG injections – Mimic LH to stimulate the testes
- Thyroid hormone therapy – For hypothyroidism
- Cabergoline or bromocriptine – To treat high prolactin levels
Hormonal therapy should be guided by blood test results and supervised by a fertility specialist.
3. Surgical Intervention (e.g., Varicocele Repair)
A varicocele—a dilated vein in the scrotum—can impair sperm production and motility due to increased heat and oxidative stress. Surgical correction (varicocelectomy) may lead to:
- Improved sperm motility
- Better sperm morphology
- Increased natural conception rates
Not all varicoceles require surgery—only those that are clinically significant and associated with abnormal semen parameters.
4. Antioxidant Supplementation
Oxidative stress is a key cause of sperm motility damage. Certain antioxidant supplements have been shown to support motility by reducing oxidative damage:
- Coenzyme Q10
- L-carnitine and acetyl-L-carnitine
- Zinc
- Vitamin C, E, and selenium
- N-acetylcysteine (NAC)
Supplementation may be especially helpful when no specific medical cause is found (idiopathic asthenozoospermia).
5. Assisted Reproductive Technologies (ART)
In cases where medical or lifestyle treatments are not sufficient, ART can help overcome low motility:
- Intrauterine insemination (IUI): May be effective in mild cases of motility issues
- In vitro fertilization (IVF): Suitable when sperm quality is moderately to severely impaired
- Intracytoplasmic sperm injection (ICSI): Recommended when sperm motility is severely reduced or total motile sperm count is very low
ICSI involves injecting a single viable sperm directly into the egg, bypassing the need for it to swim naturally.
📝 Key Takeaway:
Poor sperm motility is treatable in many cases. Identifying the root cause and working with a fertility specialist allows couples to choose the least invasive, most effective treatment path based on their individual situation.
Natural Ways to Improve Sperm Motility and Health
While medical treatment may be necessary in certain cases, many men with poor sperm motility can benefit significantly from natural lifestyle changes. A holistic approach focusing on nutrition, exercise, supplements, and healthy habits can enhance sperm quality, reduce oxidative stress, and support overall reproductive health.

🥗 1. Eat a Fertility-Friendly Diet
A balanced diet rich in vitamins, minerals, and antioxidants can improve sperm motility and reduce cellular damage:
- Zinc – Boosts testosterone and sperm development (found in oysters, beef, pumpkin seeds)
- Selenium – Helps maintain sperm structure and motility (Brazil nuts, tuna)
- Vitamin C and E – Protect sperm from oxidative stress
- Omega-3 fatty acids – Improve membrane fluidity and motility (salmon, walnuts, flaxseeds)
- Folate and B12 – Support DNA synthesis and cellular health
Avoid excessive sugar, processed foods, and trans fats, which may contribute to inflammation and hormonal imbalance.
💊 2. Consider Targeted Supplements
Certain supplements have shown promising results in boosting sperm motility:
- Coenzyme Q10 (CoQ10): Powerful antioxidant that improves mitochondrial function
- L-Carnitine & Acetyl-L-Carnitine: Support energy metabolism in sperm
- Ashwagandha: Adaptogen that may improve testosterone levels and motility
- Maca Root: Traditionally used for sexual function and energy
- Vitamin D: Low levels are associated with poor motility and fertility
Always consult with a healthcare provider before starting a supplement regimen, especially if undergoing fertility treatment.
🏃♂️ 3. Maintain a Healthy Weight and Exercise Regularly
Obesity is associated with lower testosterone, increased estrogen, and reduced sperm motility. To support hormonal balance and reproductive health:
- Aim for moderate-intensity exercise (30–45 minutes, 3–5 times per week)
- Include resistance training to boost testosterone
- Avoid overtraining, which can increase cortisol and oxidative stress
🛌 4. Improve Sleep Hygiene
Sleep is essential for hormone production, sperm regeneration, and overall health. Tips:
- Get 7–8 hours of quality sleep per night
- Maintain a regular sleep schedule
- Avoid blue light and stimulants before bed
- Address sleep disorders (e.g., sleep apnea)
Poor sleep is strongly linked to decreased fertility and testosterone levels.
🧘♂️ 5. Reduce Stress
Chronic stress elevates cortisol, which suppresses testosterone and impairs sperm production. Stress-reducing practices include:
- Meditation and deep breathing
- Yoga or tai chi
- Spending time in nature
- Creative activities and hobbies
Even 15–30 minutes of daily relaxation can make a difference.
☢️ 6. Avoid Environmental Toxins and Heat
Protect your reproductive health by limiting exposure to:
- Plastic chemicals (e.g., BPA, phthalates) – Use glass or stainless-steel containers
- Pesticides and herbicides – Wash fruits and vegetables thoroughly
- Heavy metals – Limit exposure in certain occupations
- Heat sources – Avoid hot tubs, saunas, and tight underwear
- Keep laptops and phones away from the groin area
🚭 7. Eliminate Harmful Habits
- Quit smoking – Damages sperm DNA and decreases motility
- Limit alcohol – Excessive drinking impairs hormone production
- Avoid recreational drugs – Particularly marijuana, anabolic steroids, and opioids
📌 Final Note:
Natural approaches can take 2–3 months to show measurable improvements, as sperm production follows a cycle of about 72–90 days. Consistency and patience are key.
When to See a Fertility Specialist
While many cases of reduced sperm motility can be improved with lifestyle changes and supplements, medical evaluation is crucial when the issue persists or when a couple has been trying to conceive for an extended period without success. A fertility specialist can help identify the root cause and recommend appropriate treatment options—ranging from hormonal therapy to assisted reproductive technologies (ART).
Signs That It’s Time to Seek Help
You should consult a fertility specialist if:
- You’ve been trying to conceive for 12 months or more without success (or 6 months if the female partner is over 35)
- A semen analysis shows low motility, low sperm count, or abnormal morphology
- You have a history of:
Undescended testicles (cryptorchidism)
Testicular torsion, injury, or infection (e.g., mumps orchitis)
Cancer treatments (chemotherapy or radiation)
Anabolic steroid use or testosterone replacement
- You experience symptoms of low testosterone, such as fatigue, low libido, or erectile dysfunction
- You or your partner have known reproductive or hormonal disorders
What a Specialist Can Offer
A fertility specialist (such as a reproductive urologist or endocrinologist) may recommend:
- Comprehensive semen analysis
- Hormonal testing (testosterone, FSH, LH, prolactin, thyroid)
- Genetic testing, if indicated
- Scrotal ultrasound to check for varicocele or testicular abnormalities
- Lifestyle or supplement guidance tailored to your needs
- Advanced fertility treatment options such as IUI, IVF, or ICSI
Early diagnosis and intervention significantly improve the chances of successful conception, especially when combined with the right treatment plan.
Frequently Asked Questions (FAQs)
❓ Can low sperm motility be improved?
Yes, in many cases. Sperm motility can often be improved through lifestyle changes, nutritional support, antioxidant supplements, and, when needed, medical or surgical treatment. Results typically begin to show after 2–3 months due to the sperm regeneration cycle.
❓ What is a good sperm motility percentage?
According to the World Health Organization (WHO), progressive motility ≥32% or total motility ≥40% is considered normal. Anything below these values may reduce fertility and may require further evaluation.
❓ Does poor motility mean I’m infertile?
Not necessarily. While low motility can reduce the chances of natural conception, many men with poor motility can still conceive with the help of assisted reproductive technologies (ART) such as IUI, IVF, or ICSI.
❓ How long does it take to improve sperm motility naturally?
On average, it takes about 2–3 months to see meaningful improvements, since sperm take approximately 72–90 days to develop. Consistency in lifestyle, nutrition, and supplementation is key.
❓ Can stress really affect sperm motility?
Yes. Chronic stress elevates cortisol, which can interfere with hormone production, reduce testosterone, and impair spermatogenesis. Managing stress effectively can contribute to better sperm quality.
Summary & Final Thoughts
Sperm motility is a key pillar of male fertility, influencing whether sperm can reach and fertilize the egg. While poor motility—known as asthenozoospermia—can make natural conception more difficult, it’s important to remember that it’s not the end of the road.
With proper evaluation, targeted medical treatment, and sustainable lifestyle changes, many men can improve their sperm motility and increase their chances of becoming fathers. From nutritional strategies and stress management to cutting-edge fertility technologies, the path to parenthood is more accessible than ever.
If you’re concerned about your sperm health or struggling to conceive, don’t wait. A simple semen analysis and expert guidance from a fertility specialist can provide the answers—and options—you need to move forward with confidence.





