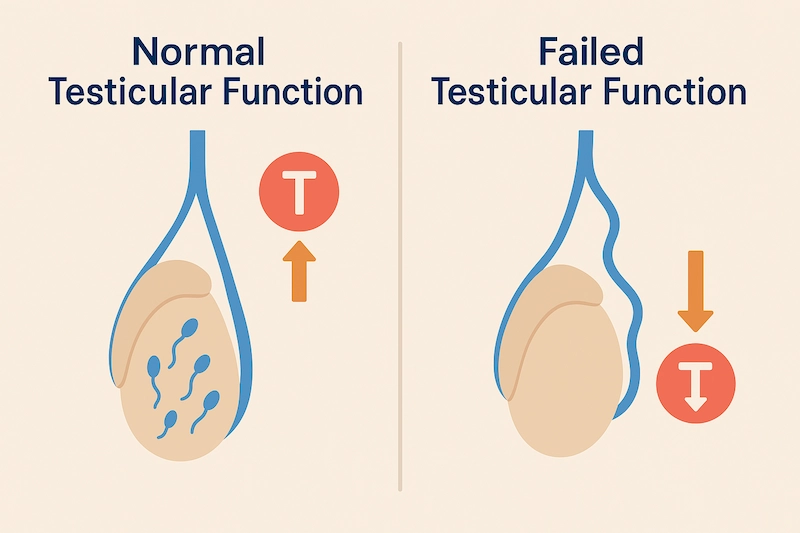
Testicular failure, also known as primary hypogonadism, occurs when the testes are unable to produce sufficient amounts of testosterone or sperm. This condition is one of the major causes of male infertility and may result from genetic factors, medical treatments, injury, or hormonal imbalances. Unlike secondary hypogonadism—which involves the brain or pituitary—testicular failure is a direct dysfunction of the testicles themselves.
For men trying to conceive, understanding the underlying causes of testicular failure and available treatment options is critical. In this article, we explore the role of the testes in male fertility, what happens when they fail to function properly, and how medical intervention, hormone therapy, or assisted reproduction may help.
What Is Testicular Failure?
Testicular failure, also known as primary testicular failure or primary hypogonadism, refers to the condition in which the testes are unable to produce adequate levels of testosterone and/or fail to generate healthy sperm. This condition significantly impairs male reproductive function and is one of the leading causes of non-obstructive azoospermia—a condition where no sperm is present in the semen due to production failure rather than a blockage.
Primary vs. Secondary Hypogonadism
It’s important to distinguish between primary and secondary hypogonadism, as they differ in origin:
- Primary hypogonadism (testicular failure): The problem lies in the testicles themselves. Despite normal or elevated levels of LH (luteinizing hormone) and FSH (follicle-stimulating hormone) from the pituitary, the testes do not respond appropriately, leading to low testosterone and impaired sperm production.
- Secondary hypogonadism: Involves a dysfunction in the hypothalamus or pituitary gland, which fails to produce adequate LH and FSH to stimulate the testes.
In testicular failure, the body may actually attempt to compensate by producing higher levels of LH and FSH, but the testes remain nonresponsive—a classic example of hypergonadotropic hypogonadism.
Key Functions Affected
When the testes fail, two main processes are impaired:
- Testosterone Production – leading to symptoms such as reduced libido, fatigue, muscle loss, and mood changes.
- Spermatogenesis – the creation and maturation of sperm cells, resulting in infertility or severely low sperm counts.
Is It Reversible?
Some cases of testicular failure are irreversible, particularly when caused by genetic disorders, radiation, or complete testicular damage. However, partial or acquired cases—due to infections, trauma, or toxins—may be partially reversible with prompt diagnosis and appropriate intervention.
Causes of Testicular Failure
Testicular failure can result from a variety of congenital (present at birth) or acquired (developed later) conditions. Understanding these underlying causes is essential for determining prognosis, treatment options, and whether fertility can be restored.
1. Genetic Disorders
Some men are born with genetic abnormalities that impair testicular development or function, including:
- Klinefelter Syndrome (47,XXY): The most common chromosomal cause of testicular failure. Affected men have small, firm testicles, low testosterone, and azoospermia.
- Y Chromosome Microdeletions: Specific deletions (especially in the AZF regions) can lead to severe oligospermia or complete absence of sperm production.
- Androgen Insensitivity Syndrome: The body cannot respond to testosterone, despite normal or high levels.
These conditions often result in irreversible infertility but may still allow for hormonal treatment to address symptoms.
2. Undescended Testicles (Cryptorchidism)
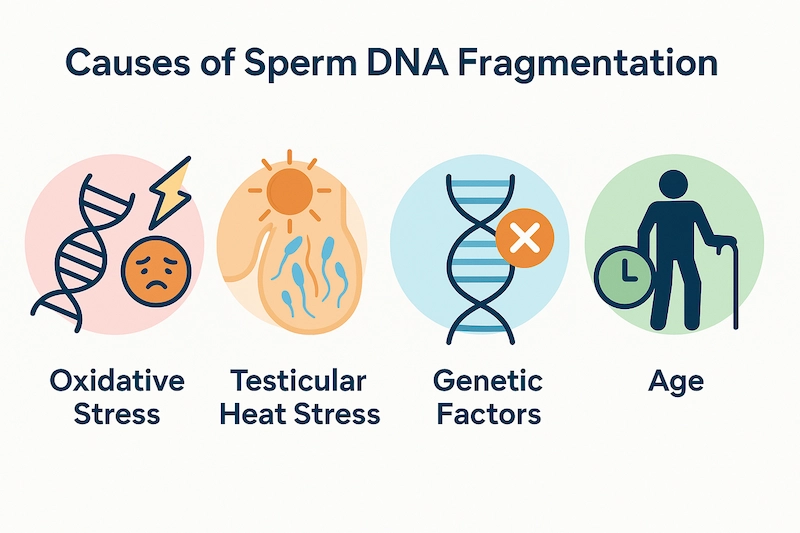
In this condition, one or both testicles fail to descend into the scrotum during infancy. If not corrected early (preferably before age 1), the retained testicle may suffer from heat damage, leading to permanent fertility issues.
Even after surgical correction (orchiopexy), some men may still experience suboptimal sperm production.
3. Testicular Torsion or Trauma
Testicular torsion, where the spermatic cord twists and cuts off blood supply, can cause irreversible damage if not treated within 6 hours. Blunt trauma (e.g., sports injuries) may also impair testicular tissue and reduce fertility potential.
These cases may lead to unilateral (one-sided) or bilateral (both sides) testicular failure.
4. Infections
Severe infections targeting the testes can destroy the sperm-producing cells:
- Mumps orchitis: A common complication of mumps virus in post-pubertal males, leading to testicular inflammation and atrophy
- STIs or systemic infections (e.g., tuberculosis) may also contribute to testicular damage
Infection-related testicular failure may be preventable through vaccination and early treatment.
5. Chemotherapy and Radiation
Cancer treatments—especially those involving alkylating agents or pelvic/abdominal radiation—can severely impair or permanently halt sperm production.
Many men become azoospermic after such therapies. Sperm banking before treatment is strongly recommended for those wishing to preserve fertility.
6. Autoimmune Conditions
In rare cases, the immune system may produce antibodies that attack testicular tissue, known as autoimmune orchitis. This leads to inflammation, fibrosis, and eventual failure of the seminiferous tubules.
This condition is difficult to reverse but may be managed with immunosuppressive therapy in select cases.
7. Environmental Toxins and Endocrine Disruptors
Long-term exposure to harmful substances may damage the testes:
- Heavy metals (lead, cadmium)
- Phthalates and BPA (found in plastics)
- Pesticides, herbicides, industrial chemicals
These agents may interfere with testosterone production or directly impair the sperm-producing cells.
Signs and Symptoms of Testicular Failure
Testicular failure can present with a combination of reproductive, hormonal, and physical symptoms. In many cases, the condition is not diagnosed until a man is evaluated for infertility or presents with signs of low testosterone.
❌ Infertility or Azoospermia
One of the hallmark signs of testicular failure is male infertility, especially when a semen analysis reveals:
- Azoospermia (no sperm in the semen)
- Severe oligospermia (very low sperm count)
- Poor sperm motility or abnormal morphology
In many cases, fertility issues are the first clue that prompts further hormonal evaluation.
📉 Low Libido and Sexual Dysfunction
Because testosterone production is often significantly reduced, men may experience:
- Decreased sexual desire (low libido)
- Difficulty achieving or maintaining erections
- Weak or absent ejaculation
These symptoms are sometimes mistaken for psychological issues or aging but are often hormonally driven.
😴 Fatigue and Low Energy
Testosterone plays a key role in energy metabolism and vitality. Men with testicular failure often report:
- Persistent fatigue
- Lack of motivation
- Poor exercise tolerance or stamina
This may affect both daily performance and emotional well-being.
💪 Loss of Muscle Mass and Increased Body Fat
Testosterone helps maintain lean muscle mass and regulate fat metabolism. Low levels can lead to:
- Decreased strength and muscle tone
- Increased abdominal or body fat
- A softer body composition over time
This can further contribute to reduced confidence and energy.
🧍♂️ Small or Firm Testicles
Testicular failure often causes changes in testicular size and texture, including:
- Smaller-than-normal testicles
- Firm or rubbery consistency on palpation
- Testicular asymmetry or shrinkage over time
These signs are often identified during a physical examination.
👦 Delayed or Incomplete Puberty (in congenital cases)
In men with congenital forms of testicular failure (such as Klinefelter syndrome), symptoms may include:
- Delayed or incomplete puberty
- Lack of body hair, muscle growth, or deepening of the voice
- Taller stature with disproportionately long limbs
These signs typically become apparent during adolescence.
🧔 Gynecomastia (Breast Enlargement)
An imbalance between testosterone and estrogen can lead to breast tissue growth in men, also known as gynecomastia. It may be associated with tenderness or swelling in the chest area.
How Testicular Failure Affects Fertility
Testicular failure directly compromises the male reproductive system’s ability to produce viable sperm, making it one of the primary causes of non-obstructive azoospermia and male infertility. It also disrupts the hormonal balance necessary for normal spermatogenesis and sexual function.
Impaired Spermatogenesis
The testes are responsible for producing sperm within the seminiferous tubules, a process heavily dependent on both FSH stimulation and functional Sertoli cells. In testicular failure, this system is impaired or completely shut down due to:
- Degeneration of germ cells
- Damage to the tubules from toxins, trauma, or genetic abnormalities
- Poor support from dysfunctional Sertoli cells
The result is severely reduced sperm production or complete absence of sperm in the ejaculate.
Reduced Testosterone Levels
Testicular failure also impairs Leydig cells, which are responsible for testosterone production. Testosterone is essential not only for sperm development but also for:
- Maintaining libido
- Supporting erectile function
- Preserving muscle mass and bone density
- Regulating mood and energy levels
Low testosterone can exacerbate the effects of infertility by further decreasing sexual function and motivation.
Disrupted Hormonal Feedback Loop
In cases of primary testicular failure, the pituitary gland continues to secrete LH and FSH in an attempt to stimulate the testes. However, because the testes cannot respond properly, these hormones remain elevated, creating a condition known as hypergonadotropic hypogonadism.
This hormonal pattern is a key diagnostic clue in distinguishing testicular failure from secondary (pituitary-based) causes.
❌ Reduced Chances of Natural Conception
Men with complete testicular failure often experience:
- Azoospermia (no sperm in the semen)
- Extremely low sperm counts that are not compatible with natural conception
- Abnormal sperm morphology or motility, when any sperm are present
In such cases, assisted reproductive technologies (ART)—such as IVF or ICSI using surgically retrieved sperm—are often required to achieve biological fatherhood.
Diagnostic Evaluation
Accurate diagnosis of testicular failure is essential for determining the cause of infertility and guiding the most appropriate treatment options. The evaluation typically involves a combination of clinical assessment, hormonal testing, semen analysis, and sometimes genetic or imaging studies.
🩺 Medical History and Physical Examination
The diagnostic process begins with a comprehensive review of medical and reproductive history, including:
- Duration of infertility
- History of cryptorchidism, mumps, trauma, or cancer treatment
- Use of anabolic steroids or testosterone therapy
- Symptoms of low testosterone (e.g., fatigue, low libido, mood changes)
- Family history of infertility or genetic conditions
During the physical exam, the physician may assess:
- Testicular size and consistency
- Presence of gynecomastia
- Body hair distribution and signs of puberty
- Varicocele or other scrotal abnormalities
🧪 Hormonal Blood Tests
Hormonal evaluation helps confirm the diagnosis and differentiate primary from secondary hypogonadism:
- Total and free testosterone – Usually low in testicular failure
- LH and FSH – Often elevated (hypergonadotropic pattern)
- Estradiol – May be elevated due to decreased testosterone
- Prolactin – To rule out pituitary causes
- TSH and thyroid hormones – To check for thyroid-related issues
- SHBG (sex hormone-binding globulin) – Helps interpret free testosterone levels
This hormonal profile is typically enough to confirm primary testicular failure.
Semen Analysis
A semen analysis is performed to evaluate:
- Sperm count (often zero or severely low)
- Motility and morphology
- Volume and pH of ejaculate
Men with azoospermia or severe oligospermia may require additional evaluation.
Genetic Testing
Genetic tests are recommended if the patient has:
- Non-obstructive azoospermia
- Small, firm testicles
- Elevated FSH with no obvious acquired cause
Common tests include:
- Karyotype analysis (to detect Klinefelter syndrome)
- Y chromosome microdeletion analysis (especially AZFa, AZFb, AZFc regions)
- CFTR gene mutation testing (if congenital absence of the vas deferens is suspected)
Imaging Studies
Imaging may be used to evaluate anatomical or internal abnormalities:
- Scrotal ultrasound – To assess testicular size, texture, and structure
- Pituitary MRI – Only if secondary hypogonadism is suspected or prolactin is elevated
Testicular Biopsy
A testicular biopsy may be indicated in certain cases to distinguish between:
- Sertoli cell-only syndrome
- Maturation arrest
- Focal areas of sperm production (which may be used for sperm retrieval in IVF/ICSI)
This is typically performed during or prior to surgical sperm extraction procedures.
Treatment Options for Testicular Failure
The treatment of testicular failure depends on several factors, including the underlying cause, presence or absence of sperm production, symptom severity, and whether the patient is attempting to conceive. While complete restoration of testicular function is rare in severe or congenital cases, many men can still benefit from symptom management, hormonal therapy, or assisted reproductive technologies (ART).
🩺 1. Treating Underlying or Reversible Causes
In some cases, testicular failure may be partially reversible, especially if it is due to:
- Infections (e.g., mumps orchitis): Early treatment may prevent permanent damage.
- Toxins or medications: Discontinuation of gonadotoxic agents (e.g., chemotherapy, certain drugs) may allow partial recovery.
- Anabolic steroid abuse: Stopping exogenous testosterone can lead to gradual recovery of natural testosterone and sperm production over months to a year.
However, most genetic or severe structural causes (e.g., Klinefelter syndrome, Sertoli-cell only syndrome) are not reversible.
💉 2. Hormone Replacement Therapy (HRT)
For men with symptoms of low testosterone—such as fatigue, low libido, muscle loss, and mood changes—testosterone replacement therapy (TRT) can significantly improve quality of life.
Common TRT options include:
- Topical gels or creams
- Intramuscular injections (e.g., testosterone enanthate or cypionate)
- Transdermal patches
- Implants or oral formulations
⚠️ Important note: TRT does not restore fertility and often suppresses sperm production by shutting down LH and FSH. Therefore, it is not suitable for men actively trying to conceive.
3. Gonadotropin Therapy (hCG ± FSH)
In men with residual testicular function or secondary testicular failure, hCG (human chorionic gonadotropin) may be used to stimulate testosterone production by mimicking LH. When combined with recombinant FSH, it may also stimulate spermatogenesis.
Indications:
- Secondary hypogonadism (especially in young men with pituitary dysfunction)
- Azoospermic men undergoing fertility treatment
This therapy requires close monitoring and can take 3–6 months or longer to see results.
🧪 4. Surgical Sperm Retrieval for ART
In men with non-obstructive azoospermia due to testicular failure, natural conception is typically not possible. However, some may still have small pockets of sperm production within the testes, allowing for surgical extraction and use in IVF or ICSI.

Techniques include:
- TESE (Testicular Sperm Extraction)
- Micro-TESE (Microsurgical TESE) – More advanced, uses microscope to identify and extract areas of active spermatogenesis
If viable sperm are retrieved, they can be injected directly into the egg during intracytoplasmic sperm injection (ICSI).
Success depends on:
- Type and severity of testicular damage
- Underlying cause (e.g., AZFc deletion has better prognosis than AZFa)
- Female partner’s fertility status
🧑🍼 5. Use of Donor Sperm
If no sperm can be retrieved (or if the man carries a serious genetic defect), couples may consider using donor sperm through:
- Intrauterine insemination (IUI)
- IVF with donor sperm
This option allows conception but does not provide genetic paternity. It may be appropriate in cases of:
- Complete spermatogenic failure
- Irreversible genetic infertility
- Repeated failed surgical sperm retrieval
Counseling and emotional support are essential when exploring this option.
🌱 6. Fertility Preservation and Future Planning
For men at risk of testicular failure (e.g., before chemotherapy, radiation, or orchiectomy), sperm banking is highly recommended. This involves collecting and freezing sperm for future use in ART.
In adolescents or young men diagnosed with early-stage testicular failure, fertility preservation discussions should occur as early as possible.
🧠 7. Psychological and Emotional Support
Testicular failure and male infertility can be emotionally distressing, affecting self-esteem, relationships, and mental health. Access to:
- Individual or couples counseling
- Support groups
- Medical education and realistic fertility planning
…can help men and their partners navigate the physical and emotional challenges more effectively.
Lifestyle and Supportive Measures
While medical and hormonal treatments are often necessary for managing testicular failure, healthy lifestyle choices can enhance overall well-being and help support any remaining reproductive potential. These supportive strategies can also improve outcomes in men pursuing fertility treatments.
🥦 1. Nutritional Support
A nutrient-rich diet can help optimize hormone metabolism, reduce inflammation, and improve general reproductive health. Recommended nutrients include:
- Zinc – Essential for testosterone production and sperm quality
- Vitamin D – Supports testicular function and hormonal balance
- Selenium – Antioxidant that protects sperm DNA and improves motility
- Omega-3 fatty acids – Found in fish, flaxseed; reduce oxidative stress
- Folate and B-complex vitamins – Support cellular health and sperm development
Limiting processed foods, sugar, and trans fats is equally important.
🏃♂️ 2. Regular Physical Activity
Exercise boosts circulation, testosterone levels, and mood. Best practices include:
- Strength training (2–4 times per week) to maintain muscle mass
- Moderate aerobic activity (e.g., brisk walking, cycling) for heart health
- Avoiding overtraining, which can increase cortisol and lower testosterone
Staying active also helps maintain a healthy weight, which is critical for hormonal health.

🛌 3. Prioritize Quality Sleep
Sleep is vital for hormone production, especially testosterone, which peaks during deep sleep. Men with testicular failure should aim for:
- 7–8 hours of uninterrupted sleep
- A consistent bedtime and wake-up schedule
- Limiting screen time and caffeine before bed
- Evaluating for sleep apnea if symptoms are present
Good sleep hygiene supports energy, mood, and metabolism.
😌 4. Manage Stress
Chronic stress raises cortisol, which disrupts the HPG axis and may worsen hormonal imbalances. Stress management techniques include:
- Mindfulness meditation or breathing exercises
- Yoga or tai chi
- Time in nature or low-intensity outdoor activity
- Support from friends, family, or professional counseling
Even 15–30 minutes of daily stress reduction can yield noticeable benefits.
☣️ 5. Avoid Environmental Toxins
Exposure to certain chemicals can negatively impact testicular function and hormone balance. Tips include:
- Use glass or stainless steel instead of plastic for food storage
- Choose BPA-free products
- Avoid pesticides and industrial chemicals when possible
- Limit use of personal care products with parabens or phthalates
These small changes help minimize endocrine disruption.
🚭 6. Eliminate Harmful Habits
Men with testicular failure should avoid substances that further impair hormonal or reproductive function:
- Quit smoking – linked to oxidative damage and sperm DNA fragmentation
- Limit alcohol – excess use affects testosterone and liver metabolism
- Avoid anabolic steroids or unregulated testosterone boosters
A healthy lifestyle cannot reverse severe testicular failure, but it can optimize the body’s response to treatment and support long-term wellness.
Prognosis and Long-Term Outlook
The prognosis for men with testicular failure varies widely depending on the cause, extent of testicular damage, and whether any sperm production remains. While full restoration of fertility is often not possible in severe or congenital cases, advances in reproductive medicine and hormonal therapy can help many men achieve parenthood or manage symptoms effectively.
Fertility Prospects
- Men with partial testicular failure may retain limited sperm production and respond to hormonal stimulation therapy, enabling natural conception or assisted reproduction.
- In cases of non-obstructive azoospermia, micro-TESE can sometimes retrieve viable sperm for use in ICSI (intracytoplasmic sperm injection).
- Men with complete spermatogenic failure (e.g., Sertoli-cell only syndrome, AZFa deletion) have no chance of biological paternity, and must consider donor sperm or adoption if they wish to build a family.
- Early sperm banking before medical treatments (chemotherapy, radiation, surgery) offers better reproductive options later in life.
Genetic Considerations
Some genetic causes of testicular failure (e.g., Klinefelter syndrome, Y-chromosome microdeletions) can be inherited or passed on through assisted reproduction.
- Genetic counseling is recommended for couples using ART, especially in cases involving male factor infertility.
- Preimplantation genetic testing (PGT) may be used during IVF to screen embryos for abnormalities if indicated.
Long-Term Hormonal Support
For men with persistently low testosterone, lifelong hormone replacement therapy (HRT) may be necessary to maintain:
- Sexual function and libido
- Bone density
- Muscle mass and strength
- Mood, memory, and energy levels
- Cardiovascular and metabolic health
Regular monitoring is essential to avoid side effects and ensure optimal hormonal balance.
🩺 Health Monitoring and Preventive Care
Men with testicular failure should have ongoing medical follow-up to assess:
- Bone density (risk of osteoporosis from low testosterone)
- Hematocrit and cardiovascular risk (in men on TRT)
- Mental health – especially in those coping with infertility or long-term hormone therapy
- Metabolic health – including weight, cholesterol, and glucose control
Emotional and Psychological Outlook
Coping with infertility and lifelong hormonal therapy can be challenging. Many men benefit from:
- Psychological counseling or therapy
- Support groups for male infertility or hypogonadism
- Open communication with partners and healthcare providers
A proactive and supported approach can help men lead fulfilling lives, even in the face of testicular failure.
When to See a Fertility Specialist
Early referral to a fertility specialist or reproductive urologist is crucial for men with suspected testicular failure, especially those trying to conceive. Prompt evaluation can help identify potentially reversible causes, preserve fertility options, and initiate appropriate treatment.
Signs That Warrant Specialist Evaluation
You should consult a fertility specialist if you experience:
- Inability to conceive after 12 months of regular, unprotected intercourse
- Low or zero sperm count on semen analysis (azoospermia or severe oligospermia)
- Symptoms of low testosterone (fatigue, low libido, erectile dysfunction, mood changes)
- Small or firm testicles noted on self-exam or physical examination
- History of:
Undescended testicles (cryptorchidism)
Mumps orchitis or testicular injury
Cancer treatments (chemotherapy or radiation)
Anabolic steroid use
Early evaluation improves the chances of successful fertility treatment or sperm preservation.
Who You Should See
Depending on your condition and goals, your care team may include:
- Urologist specializing in male infertility – for diagnostic evaluation, hormonal treatment, and surgical sperm retrieval
- Reproductive endocrinologist – if pursuing assisted reproductive technologies (e.g., IVF or ICSI)
- Genetic counselor – if a hereditary condition is suspected
- Psychologist or counselor – for emotional and relationship support
What to Expect
Your specialist may recommend:
- Comprehensive hormonal testing
- Semen analysis (or repeat testing if needed)
- Genetic screening
- Scrotal ultrasound or testicular biopsy
- Development of a personalized treatment plan based on fertility goals and test results
Timely diagnosis and care can make a significant difference in fertility outcomes and overall health. If you have any concerns about your reproductive function, don’t wait—early action opens more doors to solutions.
Frequently Asked Questions (FAQs)
❓ Can testicular failure be reversed?
It depends on the cause. Reversible cases (e.g., due to infections, toxins, or steroid use) may improve with treatment and time. However, genetic or congenital causes (e.g., Klinefelter syndrome, Sertoli-cell only syndrome) are typically irreversible. In such cases, fertility treatment or donor sperm may be needed.
❓ Can men with testicular failure still have children?
Yes, in some cases. If sperm production is partially preserved, surgical sperm retrieval (e.g., micro-TESE) combined with ICSI may lead to a successful pregnancy. If no sperm is found, donor sperm or adoption are alternative paths to parenthood.
❓ Does testosterone therapy help fertility?
No. In fact, testosterone replacement therapy (TRT) suppresses sperm production and can worsen infertility. Men wishing to conceive should avoid TRT and explore alternative treatments like Clomiphene, hCG, or FSH under medical supervision.
❓ What are the early signs of testicular failure?
Common early signs include:
- Low libido and erectile dysfunction
- Fatigue and low energy
- Infertility or low sperm count
- Small or firm testicles
- Loss of muscle mass or increased body fat
If you notice any of these, consult a healthcare provider.
❓ Is testicular failure linked to other health problems?
Yes. Chronic low testosterone from testicular failure may increase the risk of:
- Osteoporosis (bone loss)
- Depression and anxiety
- Metabolic syndrome
- Heart disease
Hormonal therapy and lifestyle adjustments can reduce these risks.
Summary & Final Thoughts
Testicular failure is a significant but often misunderstood cause of male infertility. Whether due to genetic conditions, trauma, medical treatments, or hormonal disruptions, the inability of the testes to produce adequate sperm or testosterone can profoundly impact reproductive health and overall well-being.
While full recovery of testicular function is rare in many cases, advances in hormonal therapy and assisted reproductive technologies—such as micro-TESE and ICSI—offer real hope to men wishing to become biological fathers. For those facing irreversible infertility, donor sperm and adoption remain viable and meaningful family-building options.
Importantly, men with testicular failure can lead healthy, fulfilling lives with proper diagnosis, treatment, and ongoing medical support. Addressing lifestyle factors, preserving fertility early when possible, and seeking professional guidance are all key steps in managing this complex condition.
If you or your partner are facing fertility challenges, don’t delay. Speak to a fertility specialist and explore the many tools and technologies available today. Fertility is not always a yes-or-no answer—it’s often a journey, and the earlier you begin, the more options you’ll have.





