Varicocele is a common but often overlooked condition that can significantly impact male fertility. Characterized by enlarged veins within the scrotum, similar to varicose veins in the legs, varicoceles affect sperm production and quality in many men. While often asymptomatic, this condition is one of the leading causes of male infertility. Understanding how varicoceles develop, how they affect reproductive health, and the available treatment options can help men take proactive steps toward improving fertility. In this article, we explore everything you need to know about varicocele and its relationship with male fertility.
What Is a Varicocele?
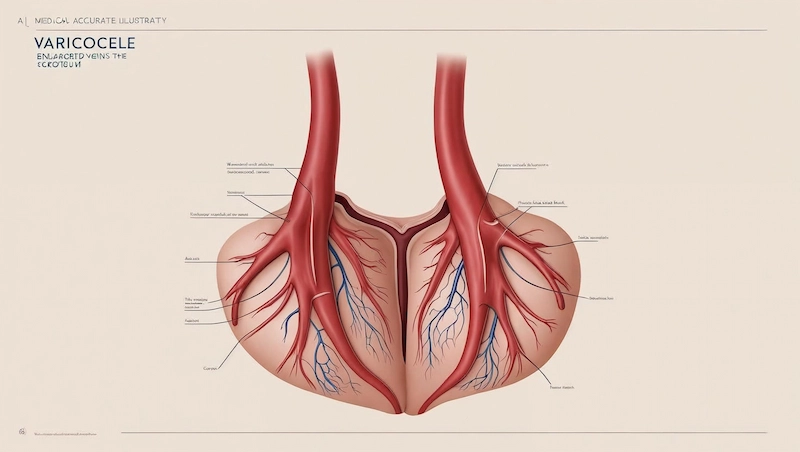
A varicocele is a medical condition characterized by the enlargement of the veins within the scrotum, specifically the pampiniform plexus, which is responsible for draining blood from the testicles. These veins become abnormally dilated due to malfunctioning valves that fail to regulate blood flow properly, resulting in blood pooling and increased pressure in the scrotal area. This condition is similar in nature to varicose veins found in the legs.
Varicoceles are most commonly found on the left side of the scrotum due to the anatomical angle of the left testicular vein as it drains into the left renal vein. However, in some cases, varicoceles may occur on both sides (bilateral), though this is less common.
The prevalence of varicocele is estimated to be around 15% of all men, and it is significantly more common in men experiencing infertility—affecting approximately 35% to 40% of men with primary infertility and up to 80% of men with secondary infertility. Most cases develop during puberty and may gradually become more noticeable over time.
Varicoceles are classified into three clinical grades based on severity:
- Grade I: Small, palpable only during Valsalva maneuver (straining)
- Grade II: Palpable without Valsalva but not visible
- Grade III: Large, visible through the scrotal skin
While many varicoceles are asymptomatic and may go unnoticed, they can have a significant impact on testicular function and fertility, especially if left untreated.
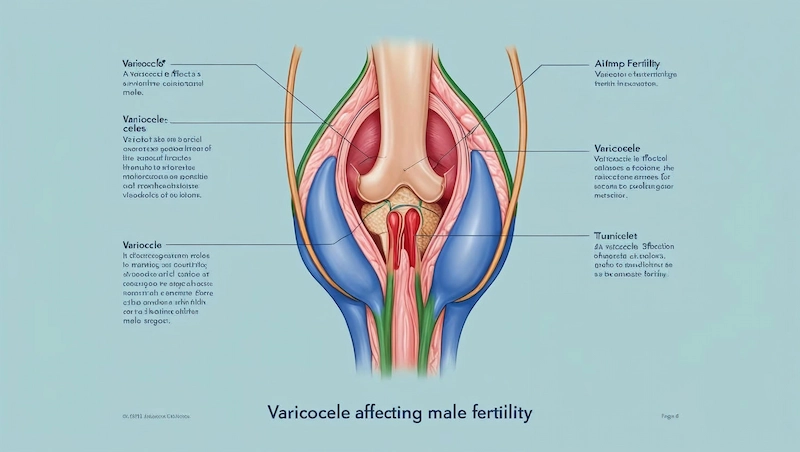
How Varicoceles Affect Male Fertility
Varicoceles are one of the most common correctable causes of male infertility. They can negatively impact testicular function and sperm parameters through several biological mechanisms. While the exact relationship between varicocele and fertility is still being researched, current medical evidence strongly supports their association with impaired reproductive potential.
Disruption of Sperm Production
One of the primary ways varicoceles affect fertility is by disrupting spermatogenesis—the process by which sperm are produced. The accumulation of warm, oxygen-poor blood in the scrotal veins creates an environment that is less than ideal for healthy sperm development. As a result, men with varicoceles often show reduced sperm count, along with poor sperm motility and morphology.
Increased Scrotal Temperature
The testicles require a temperature slightly lower than core body temperature (around 2–4°C cooler) to support optimal sperm production. Varicoceles interfere with this natural cooling system by causing blood to pool around the testicle, raising the local temperature. This thermal stress is considered a major factor in the reduction of sperm quality and function.
Oxidative Stress and DNA Damage
Men with varicoceles tend to have higher levels of reactive oxygen species (ROS) in their semen. These molecules can damage sperm by attacking cell membranes and causing DNA fragmentation. High oxidative stress is a known contributor to decreased sperm viability, reduced fertilization capacity, and increased risk of miscarriage when conception does occur.
Hormonal Imbalance
Varicoceles may also interfere with Leydig cell function—the cells responsible for producing testosterone. In some cases, this leads to subtle hormonal imbalances, including lower testosterone levels and elevated luteinizing hormone (LH) or follicle-stimulating hormone (FSH). These hormonal shifts can further impair sperm production and overall testicular health.
Testicular Shrinkage (Atrophy)
Chronic varicocele can cause testicular atrophy, where the affected testicle becomes smaller in size. This occurs due to long-term exposure to heat, poor oxygenation, and oxidative damage, all of which can damage the testicular tissue over time and reduce its function.
In summary, varicoceles create a hostile environment for sperm development by increasing scrotal temperature, causing oxidative damage, and potentially leading to hormonal and structural changes. For men struggling with infertility, identifying and treating varicocele may significantly improve their chances of natural conception.
Causes and Risk Factors of Varicocele
Understanding what causes a varicocele can help men identify their risk and seek early diagnosis and treatment. While the exact cause is not always clear, several anatomical and physiological factors are known to contribute to the development of this condition.
Valve Malfunction in Veins
The most widely accepted explanation is that varicocele results from a failure of the valves within the testicular veins (specifically, the internal spermatic veins). These valves are supposed to keep blood flowing in one direction—back toward the heart. When they become weakened or fail completely, blood pools in the scrotum, leading to vein dilation and increased pressure.
Anatomical Predisposition
Varicoceles occur more frequently on the left side due to the way the left testicular vein drains into the left renal vein at a 90-degree angle. This configuration increases pressure in the left side of the scrotum, making it more vulnerable to varicocele formation. In contrast, the right testicular vein drains more directly into the inferior vena cava.
Age and Onset During Puberty
Varicoceles typically develop during puberty, a time when the testicles grow rapidly and require increased blood flow. If the venous drainage system is underdeveloped or defective, the increased demand may overwhelm it, leading to vein enlargement. The condition is most commonly diagnosed in males between the ages of 15 and 25.
Physical Activity and Prolonged Standing
While not direct causes, activities that increase abdominal pressure, such as heavy lifting or standing for long periods, may worsen or contribute to the formation of varicoceles in individuals who are already predisposed. These factors can exacerbate venous pressure and cause symptoms to become more noticeable.
Family History
Although research is still limited, some studies suggest that genetic predisposition may play a role. Men with a family history of varicocele or venous disorders (e.g., varicose veins) may be at a higher risk of developing this condition.
Understanding these risk factors allows for better screening and preventive action, especially for men planning to start a family or experiencing fertility issues.
Signs and Symptoms of Varicocele
Many men with varicoceles may not experience any noticeable symptoms, which is why the condition often goes undiagnosed until a fertility evaluation is performed. However, in symptomatic cases, varicocele can present with a range of physical and functional signs.
⚠️ Scrotal Discomfort or Pain
One of the most common symptoms is a dull, aching pain or a feeling of heaviness in the scrotum. The pain often:
- Worsens throughout the day
- Increases after standing for long periods or physical activity
- Improves when lying down
This discomfort is due to the pressure caused by dilated veins and poor blood circulation in the testicular area.
👀 Visible or Palpable Enlarged Veins
In moderate to severe cases, a “bag of worms” appearance may be visible under the skin of the scrotum, especially when standing or straining. Upon physical examination, a healthcare provider may feel twisted, enlarged veins in the scrotum, particularly on the left side.
🔄 Asymptomatic Presentation
Up to 80% of varicocele cases are asymptomatic and may only be discovered during:
- Routine physical exams
- Fertility evaluations
- Imaging studies for unrelated issues
Although asymptomatic, these varicoceles can still affect sperm quality and testicular function, making diagnosis and monitoring important.
📉 Testicular Shrinkage (Atrophy)
In long-standing or severe cases, the affected testicle may become smaller and softer than normal. This occurs due to impaired blood flow, increased temperature, and oxidative stress, all of which damage testicular tissue over time.
Symptoms in Adolescents
In adolescents, varicoceles may not be painful but can slow testicular growth or lead to asymmetry between the two testicles. Regular check-ups are essential during puberty to monitor for early signs of varicocele-related complications.
Recognizing these symptoms and seeking medical evaluation early can help preserve fertility and prevent complications later in life.
Diagnosis of Varicocele
Diagnosing a varicocele typically involves a combination of physical examination and imaging techniques. In most cases, the condition can be identified during a routine exam, especially when a patient presents with scrotal discomfort, testicular asymmetry, or fertility concerns.
Physical Examination
The initial step in diagnosing a varicocele is a scrotal examination performed by a healthcare provider. While the patient is in a standing position, the examiner will palpate the scrotum to detect any abnormal vein dilation. In many cases, the varicocele feels like a soft mass or a bundle of twisted cords.
To enhance detection, especially for small or early-stage varicoceles, the Valsalva maneuver is often used. This involves asking the patient to bear down (as if exhaling forcefully while holding their breath), which increases abdominal pressure and can make the varicocele more prominent.
Grading of Varicocele
Varicoceles are typically classified into three grades based on their size and palpability:
- Grade I: Small varicocele, palpable only during the Valsalva maneuver
- Grade II: Moderate varicocele, palpable without Valsalva, but not visible
- Grade III: Large varicocele, easily visible through the scrotal skin
Grading helps determine the severity of the condition and whether treatment is recommended.
Scrotal Ultrasound 🖥️
A scrotal Doppler ultrasound is the gold standard imaging technique used to confirm the presence of a varicocele, especially when the physical exam is inconclusive. It provides detailed information about:
- Vein diameter (≥ 2–3 mm suggests varicocele)
- Blood flow and reflux during Valsalva maneuver
- Presence of bilateral varicoceles
Ultrasound is particularly useful in adolescents, overweight individuals, or those with subclinical varicocele—cases that are not palpable but may still impact fertility.
Additional Testing
In men undergoing fertility evaluation, a semen analysis is often ordered alongside varicocele diagnosis to assess the potential impact on sperm health. Hormonal testing may also be recommended in cases of suspected endocrine imbalance.
Early and accurate diagnosis of varicocele is essential for determining the best course of treatment and preserving male reproductive health.
Varicocele and Semen Analysis
Semen analysis is a crucial part of evaluating the impact of a varicocele on male fertility. While some men with varicoceles may have normal semen parameters, many experience abnormalities that can reduce the chances of natural conception.
Common Abnormalities in Semen Parameters
Men with varicoceles are more likely to show one or more of the following issues on a semen analysis:
- Low sperm count (oligospermia): Fewer sperm cells per milliliter of semen
- Poor sperm motility (asthenozoospermia): Reduced ability of sperm to swim effectively
- Abnormal sperm morphology (teratozoospermia): High percentage of sperm with irregular shape or structure
- Low semen volume: Occasionally observed, though less common
These factors combined can significantly impair fertilization potential, especially in moderate to severe varicocele cases.
DNA Fragmentation and Oxidative Stress 🔬
In addition to traditional semen parameters, men with varicoceles may have elevated sperm DNA fragmentation, which refers to breaks or damage in the genetic material of the sperm. This can be measured using specialized tests such as:
- SCSA (Sperm Chromatin Structure Assay)
- TUNEL assay
- Comet assay
High DNA fragmentation has been associated with reduced fertilization rates, poor embryo quality, and higher miscarriage risk after conception—either naturally or via assisted reproduction.
Oxidative stress caused by excess reactive oxygen species (ROS) in the semen is one of the key contributors to DNA damage. Identifying and addressing oxidative stress is therefore important in the management of varicocele-related infertility.
When to Perform a Semen Analysis
A semen analysis is usually recommended in the following situations:
- Infertility evaluation after 12 months of unprotected intercourse
- Prior to varicocele surgery or embolization
- Monitoring recovery after treatment
- Suspected subclinical varicocele or unexplained fertility issues
A single semen analysis provides useful information, but at least two tests spaced a few weeks apart are recommended for accuracy due to natural fluctuations in sperm quality.
Semen analysis not only helps confirm the functional impact of a varicocele but also guides decisions about treatment and fertility planning.
Treatment Options for Varicocele
Not all varicoceles require treatment. In many cases, especially when the condition is asymptomatic and fertility is not a concern, medical intervention may not be necessary. However, when a varicocele causes pain, testicular atrophy, or infertility, treatment should be considered to restore testicular function and improve reproductive outcomes.
When Is Treatment Necessary?
Treatment is typically recommended in the following situations:
- Infertility: When a couple has been trying to conceive for over 12 months and no other cause has been identified
- Abnormal semen analysis: Especially with low sperm count, motility, or morphology
- Testicular pain or discomfort: Persistent or worsening scrotal pain affecting quality of life
- Testicular atrophy: Shrinkage of the affected testicle
- Adolescents with impaired testicular growth: To prevent long-term fertility issues
Surgical Treatment: Varicocelectomy 🏥
The most common and effective treatment for varicocele is varicocelectomy, a surgical procedure that involves tying off or removing the dilated veins to redirect blood flow through normal veins.
There are several surgical approaches:
- Microsurgical subinguinal varicocelectomy: The gold standard method, performed using a microscope for precision. It has the highest success rates and lowest complication risks.
- Inguinal and retroperitoneal approaches: Older techniques with higher risk of recurrence and hydrocele formation.
- Laparoscopic varicocelectomy: Minimally invasive, done through small abdominal incisions with a camera and instruments.
Success rates are high, with improvements in semen quality seen in 60–70% of men, and spontaneous pregnancy rates ranging from 30–50% within the first year post-surgery.
Non-Surgical Treatment: Percutaneous Embolization 🩻
Percutaneous embolization is a less invasive, outpatient procedure performed by an interventional radiologist. A catheter is inserted through a vein (usually in the groin or neck) and guided to the affected testicular vein, where coils or a sclerosing agent are used to block abnormal blood flow.
Benefits include:
- No incisions or general anesthesia
- Shorter recovery time
- Can be used when surgery is high-risk or not preferred
However, this method may have a slightly higher failure and recurrence rate compared to microsurgery.
Recovery and Prognosis
Most men can return to light activities within a few days and resume normal activity within 1–2 weeks post-surgery. Pain typically improves quickly, and semen parameters begin to improve within 3–6 months.
Recurrence rates vary by method:
- Microsurgical: <5%
- Laparoscopic: 10–15%
- Embolization: 10–20%
Treatment is generally safe and effective, and many men experience significant improvements in both fertility and quality of life after intervention.
Varicocele Treatment and Fertility Outcomes
Treating a varicocele can significantly improve male fertility, especially in men with abnormal semen parameters and otherwise unexplained infertility. While not every man will achieve natural conception after treatment, numerous studies have demonstrated real improvements in sperm quality and pregnancy rates following intervention.
Improvements in Semen Quality
After varicocele repair—particularly through microsurgical varicocelectomy—many men experience measurable improvements in semen parameters such as:
- Sperm concentration
- Motility (movement)
- Morphology (shape and structure)
These improvements usually begin to appear 3 to 6 months after treatment, with the greatest benefit seen in men who had moderate abnormalities before surgery. However, men with extremely low sperm counts may experience less dramatic changes.
Natural Pregnancy Rates 👶
Studies show that 30–50% of couples achieve spontaneous pregnancy within one year following varicocele repair, depending on factors such as:
- Age of the female partner
- Duration of infertility
- Initial semen quality
- Type of surgical approach
Microsurgical varicocelectomy consistently yields the highest pregnancy success rates among treatment options.
Assisted Reproductive Technology (ART) and Varicocele
For couples undergoing intrauterine insemination (IUI) or in vitro fertilization (IVF), treating a varicocele beforehand can improve outcomes by enhancing the quality of sperm used in these procedures.
In cases where intracytoplasmic sperm injection (ICSI) is required—typically for severe male factor infertility—varicocele treatment may reduce the need for invasive ART and improve embryo quality.
Even if natural conception does not occur, post-treatment improvements may allow couples to use less intensive and less costly fertility treatments.
Impact on Hormonal Balance and Testosterone
Some studies also suggest that varicocele repair can lead to increased testosterone levels, especially in men with borderline low levels before treatment. This can positively influence not only fertility but also energy, libido, and overall sexual function.
Predictors of Positive Outcomes
The likelihood of fertility improvement is higher in men who:
- Have clinical varicocele (Grade II or III)
- Exhibit abnormal semen analysis
- Have normal female partner fertility
- Undergo microsurgical repair
While treatment is not a guaranteed solution for all cases of male infertility, it often represents a cost-effective and low-risk intervention that can enhance natural conception or improve the success of assisted reproduction.
Varicocele in Adolescents and Young Men
Varicoceles commonly develop during adolescence, typically between the ages of 15 and 19, when the testicles undergo rapid growth. While many adolescent varicoceles are asymptomatic and do not require immediate treatment, early detection is essential to prevent long-term complications, especially related to fertility.

Why Varicocele Occurs During Puberty
During puberty, increased blood flow to the testicles supports their growth and hormonal activity. However, if the venous valves responsible for directing blood out of the scrotum are weak or defective, this increased pressure can lead to vein dilation—resulting in a varicocele.
Impact on Testicular Growth and Development ⚠️
In adolescents, one of the most concerning effects of varicocele is testicular growth arrest or asymmetry. This occurs when the affected testicle does not grow at the same rate as the opposite side, often due to impaired blood flow and elevated scrotal temperature.
Signs to watch for include:
- A noticeable size difference between the two testicles
- Dull aching pain, especially after standing or exercise
- Reduced performance in sports or physical activity due to discomfort
When Is Treatment Recommended in Adolescents?
Treatment is usually considered if one or more of the following criteria are present:
- Testicular asymmetry > 20%
- Persistent pain or discomfort
- Bilateral varicocele
- Evidence of progressive testicular damage on follow-up exams or imaging
- Family history of infertility or concern for future fertility
Microsurgical varicocelectomy is the preferred option for adolescents requiring treatment, as it minimizes complications and recurrence.
Monitoring and Follow-up
For adolescents with small or asymptomatic varicoceles, a “watchful waiting” approach may be appropriate. This includes:
- Regular physical exams
- Scrotal ultrasound to monitor testicular size and blood flow
- Annual assessments of testicular volume and function
Early detection and appropriate management help preserve normal testicular growth and reduce the risk of infertility in adulthood.
Lifestyle and Management Tips for Men with Varicocele
While medical or surgical treatment may be necessary for some men, lifestyle modifications can also play an important role in managing varicocele symptoms, supporting testicular health, and potentially improving fertility outcomes.
🥗 Eat an Antioxidant-Rich Diet
A diet high in antioxidants helps combat oxidative stress, a known contributor to sperm DNA damage in men with varicocele. Include foods rich in:
- Vitamin C (oranges, berries, bell peppers)
- Vitamin E (almonds, sunflower seeds, spinach)
- Zinc (pumpkin seeds, oysters, beef)
- Selenium (Brazil nuts, tuna, eggs)
- Coenzyme Q10 (salmon, mackerel, whole grains)
These nutrients can support healthy sperm production and protect against cellular damage.
💊 Consider Supplements (with medical guidance)
Some studies suggest that men with varicocele-related fertility issues may benefit from supplements such as:
- L-Carnitine: Supports sperm motility
- CoQ10: Improves sperm concentration and function
- Folic acid and Zinc: Enhances sperm count
- Omega-3 fatty acids: Anti-inflammatory and supports sperm morphology
Always consult a healthcare provider before starting any supplement regimen.
❄️ Avoid Excessive Heat Exposure
Testicles require a cooler environment than the rest of the body to produce healthy sperm. To avoid scrotal overheating:
- Do not use hot tubs or saunas frequently
- Avoid tight underwear; choose loose, breathable fabrics
- Take breaks from sitting for long periods
- Avoid placing laptops or heated devices directly on the lap
🧘 Manage Stress and Sleep
Chronic stress can negatively affect hormone balance and sperm health. Incorporate stress-reduction techniques such as:
- Meditation or mindfulness
- Deep breathing exercises
- Regular physical activity
- Prioritizing 7–9 hours of quality sleep
Good sleep and emotional well-being also support healthy testosterone levels.
🏋️ Exercise, But Avoid Overstraining
Moderate exercise improves blood flow and hormonal balance. However, men with varicocele should:
- Avoid heavy weightlifting or intense abdominal pressure
- Choose low-impact activities like walking, swimming, or cycling (with a proper seat)
- Stay hydrated and avoid excessive caffeine or alcohol
🚭 Eliminate Harmful Habits
- Quit smoking: Linked to reduced sperm quality and increased oxidative stress
- Limit alcohol: Excessive drinking affects testosterone and fertility
- Avoid anabolic steroids: These can suppress natural testosterone and sperm production
By adopting these habits, men can support testicular health, improve fertility outcomes, and possibly reduce the severity or progression of varicocele symptoms—whether undergoing treatment or not.
When to See a Doctor
Although varicoceles are often harmless and asymptomatic, there are specific signs and situations when seeking medical evaluation is crucial. Early consultation with a healthcare provider can help prevent long-term complications, especially related to fertility and testicular function.
🚨 Red Flags That Require Medical Attention
You should see a doctor if you experience any of the following:
- Scrotal pain or discomfort that persists or worsens over time
- A visible or palpable mass in the scrotum that resembles a “bag of worms”
- Noticeable difference in testicle size, especially if one testicle appears smaller
- Difficulty conceiving after 12 months of regular, unprotected intercourse
- Testicular swelling, heaviness, or changes in scrotal appearance
- Symptoms worsening with physical activity or prolonged standing
- These could indicate a varicocele or another underlying condition affecting the reproductive system.
👦 Special Considerations for Adolescents
Parents or guardians should bring adolescents to a healthcare provider if:
- There’s a visible lump or asymmetry in the scrotum
- The teen complains of dull testicular pain
- Annual check-ups show slower testicular growth on one side
Early detection during puberty helps preserve future fertility and supports healthy testicular development.
🧑⚕️ What to Expect During the Evaluation
A typical varicocele evaluation includes:
- Physical examination while standing
- Valsalva maneuver to detect small or hidden varicoceles
- Scrotal ultrasound if confirmation is needed
- Semen analysis in cases of infertility
- Hormonal tests if low testosterone or other signs of hormonal imbalance are suspected
Getting evaluated early allows for better treatment planning and prevents complications like testicular atrophy or declining sperm quality.
🕒 Don’t Delay Care
Even if symptoms seem mild, untreated varicoceles may worsen over time or silently impair fertility. If you have any concerns—whether it’s discomfort, testicular changes, or fertility struggles—scheduling a urology consultation is a smart and proactive step.
Frequently Asked Questions (FAQs)
Can varicocele go away on its own?
No. Varicoceles do not go away on their own. Once the veins have become enlarged due to valve failure, the condition tends to remain stable or slowly progress over time. In some cases, symptoms may improve with lifestyle adjustments, but medical or surgical treatment is required to fully correct the condition.
Is surgery always required for varicocele?
Not always. Many varicoceles are asymptomatic and may not require treatment, especially if fertility is not a concern. Surgery or embolization is usually recommended only when the varicocele causes discomfort, testicular shrinkage, or impaired fertility.
Can I still father children if I have a varicocele?
Yes. Many men with varicoceles can father children naturally, especially if the condition is mild. However, in cases of moderate to severe varicocele—especially those affecting sperm quality—fertility may be reduced. Treating the varicocele often improves sperm parameters and increases the chances of natural conception.
What is the best treatment option for varicocele?
The most effective and commonly recommended treatment is microsurgical varicocelectomy, which has high success rates and low complication risks. However, percutaneous embolization is a less invasive alternative for those who prefer non-surgical intervention. The choice depends on individual needs, fertility goals, and medical history.
How long does recovery take after varicocele treatment?
Most men recover from varicocele surgery within 1 to 2 weeks, although full healing and improvement in semen quality may take 3 to 6 months. For embolization, recovery is usually quicker, with many men resuming normal activity in just a few days.
Can varicocele come back after treatment?
Yes, recurrence is possible but depends on the treatment method:
- Microsurgical repair has the lowest recurrence rate (under 5%)
- Laparoscopic or open surgery may have higher recurrence (up to 15%)
- Embolization has recurrence rates of 10–20%
Choosing an experienced provider and the appropriate technique minimizes the risk of recurrence.
Summary & Final Thoughts
Varicocele is a common and often underdiagnosed condition that can significantly affect male fertility by impairing sperm production, increasing scrotal temperature, and inducing oxidative stress. While many cases are asymptomatic, varicoceles are a leading cause of male infertility, particularly in men with no other identifiable reproductive issues.
Early detection—especially during adolescence or fertility evaluations—can prevent long-term damage. Fortunately, effective treatment options exist, including microsurgical varicocelectomy and percutaneous embolization, both of which can improve sperm quality and increase the chances of natural conception.
In addition to medical intervention, men with varicocele can take proactive steps to support their reproductive health by:
- Adopting a healthy, antioxidant-rich diet
- Avoiding excessive heat and physical strain
- Managing stress and lifestyle factors
If you’re experiencing scrotal discomfort, have noticed changes in testicle size, or are facing fertility challenges, don’t hesitate to consult a urologist. Addressing varicocele early can make a meaningful difference in your reproductive future and overall quality of life.